Toxin That Leads to Tetanus May Offer Way of Treating SMA
The toxin that causes tetanus may offer a way of treating spinal muscular atrophy (SMA), according to preliminary results of a study in mice, an important finding because currently there are no effective treatments for this hereditary childhood disease. The results also justify further experiments to better understand the therapeutic mechanism at play.
What’s known as tetanus toxin is a protein produced by the bacteria Clostridium tetani, and is cause of the fatal — if untreated — disease characterized by painful and uncontrollable muscle contractions. Previous studies have shown that a non-toxic sub-unit of the protein, called TTC for tetanus toxin heavy chain, may have neuro-protective properties.
In the study, “Neuroprotective Effect of Non-viral Gene Therapy Treatment Based on Tetanus Toxin C-fragment in a Severe Mouse Model of Spinal Muscular Atrophy,” published in the scientific journal Frontiers in Molecular Neuroscience, the team of Dr. Rosario Osta investigated whether TTC might have a therapeutic role in SMA.
Researchers first analysed the effect of TTC in vitro, and demonstrated that it enhances the expression of SMN, the protein that is produced in insufficient amount in SMA patients.
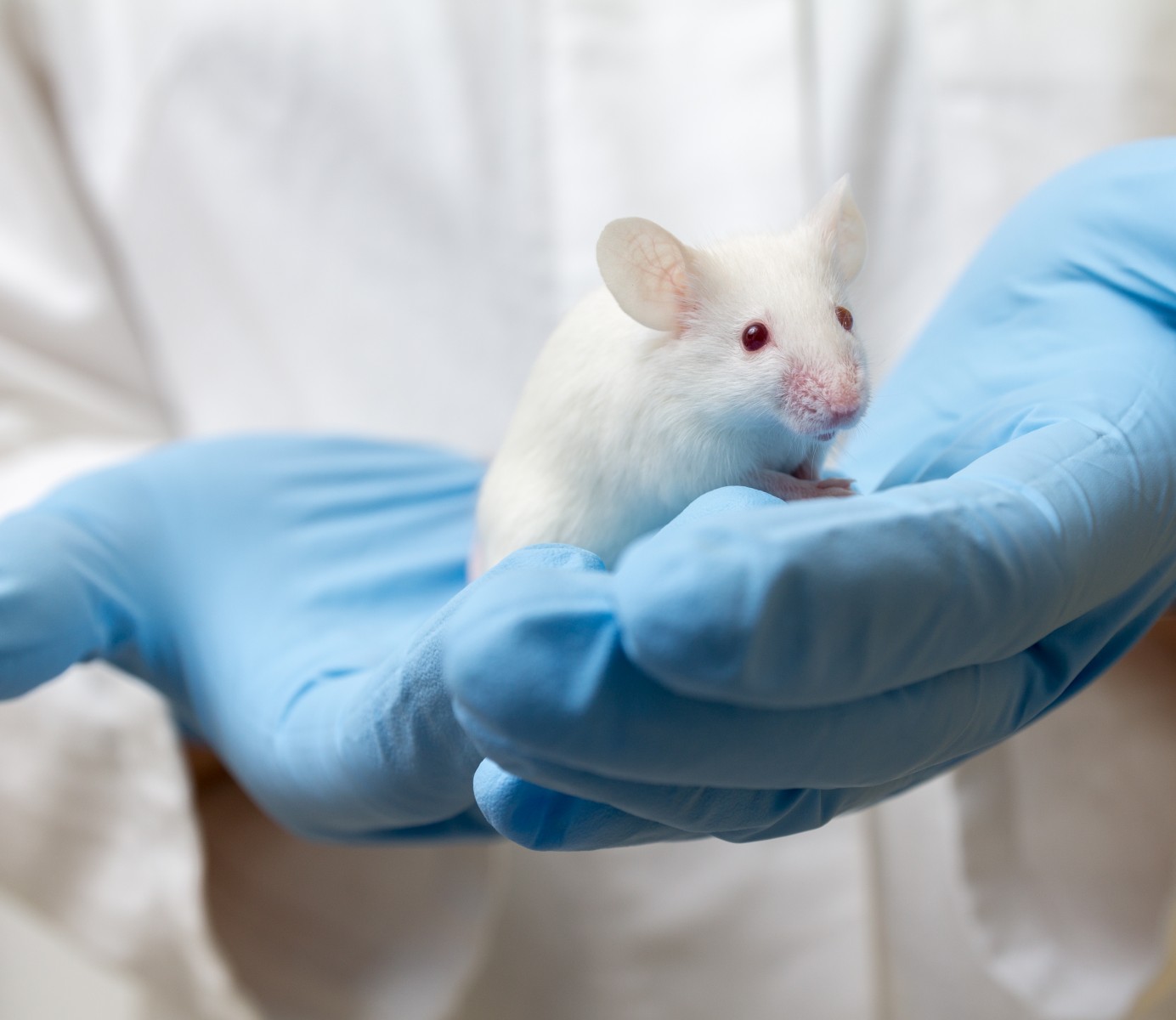
They then analysed the effect of TTC in the spinal cord and skeletal muscles of a mouse model of severe SMA.
The scientists observed that when they injected a DNA encoding for TTC into the muscle of these mice, the expression of proteins involved in autophagy, or self-degradation and cell death, was lower in the spinal cord and the skeletal muscles.
Moreover, TTC had a compensatory effect on the expression of genes involved in muscle damage response, oxidative stress, and calcium balance.
“These preliminary findings provide new insights into the effect of TTC in the spinal cord and the skeletal muscle tissues in SMA disease and suggest the need for further experiments to accurate study the effect of TTC in this disorder,” the study’s first author, Dr. Sara Oliván of Universidad de Zaragoza in Spain, and colleagues concluded.
SMA, which is caused by a mutation in the SMN1 gene, is associated with reduced levels of functional SMN protein. The most striking feature of the disease is the loss of motor neurons, which results in progressive paralysis. Being able to keep motor neurons alive would be a tremendous advance in the fight against SMA.