Protein Independent of SMN May Be Worthy Target as Combo Treatment for SMA, Mouse Study Suggests
Lowering the levels of a protein called CHP1, together with Spinraza (nusinersen) treatment, may help to improve responses to therapy in spinal muscular atrophy (SMA) patients, a study in a mouse model of the disease suggests.
Because CHP1 is independent of the survival motor neuron (SMN) protein — whose deficiency or lack of results in SMA — it may represent a new target to be used in combination with other SMA therapies.
The study, “CHP1 reduction ameliorates spinal muscular atrophy pathology by restoring calcineurin activity and endocytosis,” was published in the journal Brain.
Most lines of research into potential SMA therapies have focused on one main approach: increasing the levels of functional SMN protein, as SMN insufficiency is responsible for this disease.
Currently, the only approved treatment for SMA — Biogen‘s Spinraza — works by increasing the ability of the SMN2 gene to produce a full-length and functional SMN protein. However, many studies in SMA-affected individuals and animal models indicate that several other proteins and cellular pathways, independent of SMN, also influence the disease.
Evidence exists that manipulating the levels of these components may be a therapeutic approached, one used in combination with SMN-targeted therapies.
Researchers at the University of Cologne, Germany, looked into the mechanisms behind one such SMN-independent player, a protein called plastin 3 (PLS3), recently found to be a strong protective factor against SMA.
Increased levels of PLS3 were seen to protect children, with similar mutations in the SMN1 gene as their siblings, from developing SMA. The protective effect of PLS3 has been verified in multiple experimental models of the disease, with animals recovering from SMA symptoms when the protein is overexpressed.
The team found that PLS3 interacts with another protein called calcineurin-like EF-hand protein 1 (CHP1) — a calcium-binding protein involved in different cellular processes, including transport within cells and gene expression. Gene expression is the process by which information in a gene is synthesized to create a working product, like a protein.
CHP1 is abundant in the central nervous system at locations particularly relevant for SMA, including the growing tips of motor neurons and neuromuscular junctions — the points of contact between muscular neurons (nerve cells) and muscles.
The SMA News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
In mouse models of SMA, this protein is produced at higher-than-normal levels, suggesting it plays a role in the disease.
Importantly, lowering CHP1 levels in SMA mice successfully recovered the ability of motor neurons to grow.
Combining a Spinraza-like treatment while lowering CHP1 levels led to a 60% improvement in animals’ lifespan, compared to those given Spinraza-like treatment alone.
CHP1 reduction also contributed toward improved muscle electrical impulses, increased the size and maturation of neuromuscular junctions, and the size of muscle fibers.
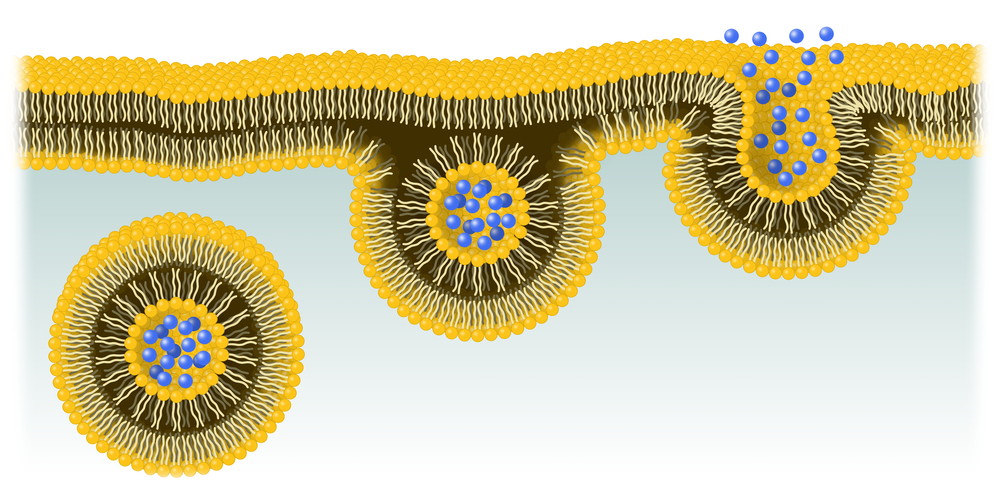
Molecular analysis suggested that CHP1 and PLS3 work together in a cellular process called endocytosis — a pathway used by cells to transport molecules. This process is paramount for the communication between motor neurons and muscles, and defects in endocytosis are though to contribute to SMA.
Reducing CHP1 levels rescued endocytosis defects in motor neurons of SMA mice. As such, researchers hypothesize that lowering CHP1 helps reduce SMA symptoms by partly restoring a normal endocytosis process.
“[W]e demonstrate that CHP1 reduction is a promising SMN-independent therapeutic target for a combinatorial SMA therapy,” they wrote.
This approach may also be beneficial for other neurodegenerative diseases, since defects in endocytosis are also present in diseases such as Parkinson’s and amyotrophic lateral sclerosis (ALS).