Neurofilament Blood Levels Likely to Predict Treatment Response in SMA
In infants with spinal muscular atrophy (SMA) type 1, lower blood levels of phosphorylated neurofilament heavy chain (pNF-H) — a marker of nerve cell damage — before starting treatment with Spinraza (nusinersen) are significantly associated with greater motor gains over time.
These findings, based on data from the Phase 3 ENDEAR trial and the SHINE extension study, contrast with those previously reported for children with types 2 and 3 disease, in whom higher pNF-H blood levels at treatment start (baseline) in trials were linked to greater motor improvements.
Still, all these results support the use of baseline pNF-H levels to predict clinical responses in SMA patients, which may differ between early and later-onset disease due to distinct age, disease duration, and remaining pool of motor neurons, the researchers suggested.
The findings were presented at the World Muscle Society (WMS) 2021 Virtual Congress, held Sept. 20–24, in the poster presentation “Phosphorylated Neurofilament Heavy Chain Level is Associated with Future Motor Function in Nusinersen-treated Individuals with Infantile-onset SMA.”
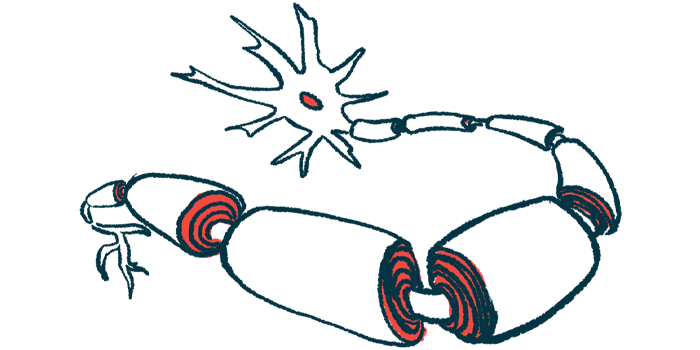
Major structural proteins of neurons, neurofilaments consist of three main subunits: heavy, intermediate, and light chains. When neurons are damaged or die, these structural proteins are released into the bloodstream and cerebrospinal fluid, the liquid that surrounds the brain and spinal cord.
As such, neurofilaments have been studied as potential biomarkers of nerve cell damage and treatment responses in people with neurodegenerative conditions, such as SMA.
A previous study showed that SMA patients in Spinraza trials had higher pNF-H levels than healthy individuals, and that these levels were rapidly and sustainably reduced after treatment.
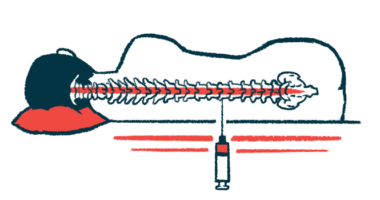
Given directly into the spinal canal every four months, Biogen’s Spinraza works by increasing the levels of SMN, a key protein for motor neuron and muscle health and whose production is impaired in SMA. It was the first disease-modifying therapy approved for SMA.
Now, Biogen and researchers involved in the Spinraza trials investigated whether baseline blood pNF-H levels could predict motor function gains with Spinraza in infants with SMA type 1, a severe and early onset disease type.
They analyzed data from the 61 infants with available, pre-treatment pNF-H levels who participated in the Phase 3 ENDEAR trial (NCT02193074), and subsequently transitioned to the ongoing SHINE open-label extension study (NCT02594124).
ENDEAR tested Spinraza against a sham procedure in 122 type 1 infants, up to 7 months old, while SHINE, expected to end in August 2023, is assessing the therapy’s long-term safety and efficacy in patients across various Spinraza trials.
The infants’ motor function was assessed with the Hammersmith Infant Neurological Examination Section 2 (HINE-2) and the Children’s Hospital of Philadelphia Infant Test of Neuromuscular Disorders (CHOP-INTEND), in which higher scores indicate better function.
HINE-2 assesses motor milestones in infants between 2 months and 2 years of age, while CHOP-INTEND evaluates motor skills of type 1 patients from 1 to over 3 years of age.
Infants’ median age at symptom onset was 1.4 months (range, 0.5–4.1 months), and they received their first Spinraza’s dose at a median of 4.9 months old (range, 1.7–8 months). They were followed for median of 3.8 years, up to five years.
Available post-Spinraza assessment timepoints ranged from day 302 (about nine months) to day 578 (about 1.5 years) for HINE-2, and from day 302 to day 1,298 (3.5 years) for CHOP-INTEND. A total of 32 patients completed all HINE-2 assessments, while 28 completed all of CHOP-INTEND’s.
After adjusting for infants’ age and motor function at baseline, lower blood pNF-H levels were found to associate with greater motor improvements (in both tests) over time.
Notably, these associations reached statistical significance at all available HINE-2 timepoints (between nine months and 1.5 years), and at 1.5 years and thereafter for CHOP-INTEND.
Similar trends were observed when analyses were restricted to patients with data available at all timepoints.
These results differ from those previously reported among Spinraza-treated children with SMA types 2 and 3 — who were 2 to 12 years old when enrolled in the Phase 3 CHERISH trial (NCT02292537) — “showing that higher baseline [blood] pNF-H was associated with greater improvements in motor function,” the researchers wrote.
As such, “the relationship between pretreatment pNF-H levels and future motor function is likely complex, depending on patient characteristics, including age and disease duration, and the remaining motor neuron pool,” they added.
“These findings inform future investigations evaluating [neurofilaments] as a predictive biomarker of treatment response in SMA,” the researchers concluded.
Biogen also announced that it is working to identify potential biomarkers in SMA, and that changes in neurofilament levels has been added as an exploratory goal to ongoing SMA studies.