Cure SMA Awards Johns Hopkins Researcher $140,000 to Study Axons in SMA
Written by |

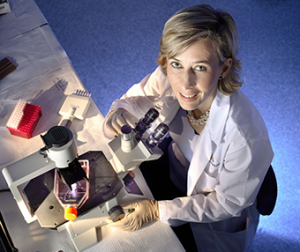
Johns Hopkins University researcher Dr. Charlotte Sumner, M.D., has been granted a Cure SMA award of $140,000 for her project, “Assessing the reversibility of proximal axon abnormalities in SMA mice.”
Sumner is a specialized adult neurologist with training in neuromuscular disease and spinal muscular atrophy (SMA) patient care. She became an SMA researcher during a fellowship at the National Institutes of Health under the mentorship of Kenneth Fischbeck, when she attended her first Cure SMA meeting in 2002 and decided to permanently switch her focus to SMA.
Sumner is currently serving as the head of a research lab focused on understanding the defects leading to SMA, and developing treatments for the condition.
“Our objective is to further characterize how the loss of SMN protein causes axonal defects in motor neurons, and to determine whether and when during development they can be reversed by SMN2 splice‐switching oligonucleotides, like nusinersen,” Sumner said in a press release.
Axons are long projections that grow out of motor neurons, sending information to other neurons or muscles. In spinal muscular atrophy patients, these axons seem to be damaged early on, due to the loss of survival of motor neuron (SMN) protein, caused by the SMN1 gene mutation.
Sumner will study how and under which circumstances these axons are damaged and whether such damage can potentially be fixed by oligonucleotides.
“Oligonucleotides are small snippets of synthetic genetic material that bind to ribonucleic acid (RNA). In SMA, they can be used to fix the splicing of SMN2, the SMA ‘backup gene,’ meaning that SMN2 would be able to make a complete SMN protein. One example of this is the drug nusinersen, being developed by Biogen and Ionis Pharmaceuticals,” Sumner said.
The team is using mouse models to further define this axonal pathology over the course of time, as well as its relationship with motor neuron death, by counting the number of axons at different prenatal and postnatal checkpoints. In previous studies, Sumner’s team found that impairments in motor axonal development during fetal and early postnatal stages of development might be key drivers of early muscle weakness and triggers of motor neuron death.
The team is also testing whether prenatally delivered SMA therapeutics could prevent these pathologies, and Sumner and her team are evaluating novel mechanisms that might regulate SMN expression and could serve as novel therapeutic targets for SMA.
“It is unknown how SMN protein deficiency causes dysfunction and ultimately death of motor neurons. This has severely limited the ability to identify non‐SMN therapeutic targets. We anticipate that these studies will provide important insights regarding the earliest functional and cellular abnormalities of SMN‐deficient motor neurons, which might then be amenable to novel therapeutic interventions and guide optimal timing for therapeutic intervention,” Sumner added.