Damage That Marks SMA Type 3 and 4 Linked to Atrophy in Neck Area of Spinal Cord, Study Reports
Later-onset forms of spinal muscular atrophy (SMA) are linked to extensive atrophy in the cervical spinal cord, particularly in gray matter of the vertebrae, that may begin long before symptoms are evident, researchers report.
The study, “The spinal and cerebral profile of adult spinal-muscular atrophy: A multimodal imaging study,” was published in NeuroImage: Clinical.
SMA, a genetic neurodegenerative disorder characterized by the gradual loss of motor neurons — the nerve cells responsible for controlling voluntary muscles — in the spinal cord and by muscular weakness. It is divided into subtypes (ranging from type 0 to type 4) depending on the age of disease onset and symptom severity.
SMA type 3 and 4 are slowly progressing forms that usually affect lower motor neurons (LMNs) — those that run from the spinal cord to the muscles. But studies in animal models have suggested that both disease forms may affect more than LMNs, and include the central nervous system.
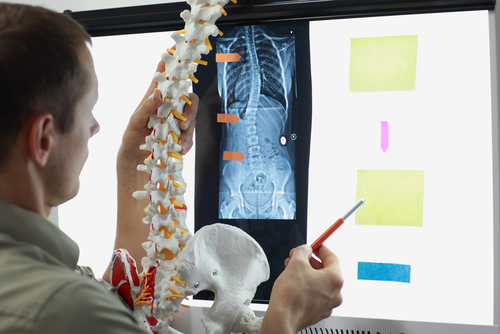
Researchers characterized the extent of spinal cord and brain lesions in type 3 and 4 adults using multimodal quantitative imaging — a technique that involves anatomy details acquired with two different image modalities (like CT scans and MRI or PET scans) to provide complementary information about what is visualized.
A total of 25 patients — 19 diagnosed with SMA type 3 and six with SMA type 4; 18 ambulant and seven non-ambulant — and 25 sex- and age-matched healthy controls were evaluated.
Ask questions and share your knowledge of SMA in our forums.
Analyses included structural measures of gray and white matter volume and white matter integrity in the spinal cord and cortical thickness, and gray matter density and white matter alterations in the brain.
Gray matter refers to areas of the central nervous system (brain, brainstem and cerebellum) made up of neuron cell bodies, while white matter refers to areas of the central nervous system made up of myelinated nerve segments (axons) responsible for the transmission of nerve signals and that connect various gray matter areas.
Researchers observed a substantial reduction of gray matter volume in the spinal cord between cervical (neck) vertebrae C3-C5 in SMA patients compared to healthy controls. No significant differences in white matter volume were found between the two groups.
Imaging analysis of the brain, however, revealed an increase in gray matter density in regions associated with motor control, which the researchers suggested could be “explained as compensatory mechanism” as a consequence of “progressive LMN degeneration.” As in the spinal cord, no significant changes in brain white matter were found.
“Spinal atrophy seems to be primarily driven by GM [grey matter] degeneration … Despite sample size limitations, our findings suggest that mechanisms underlying MN [motor neuron] degeneration in SMA are different from those taking place in other MNDs [motor neuron diseases], such as ALS [amyotrophic lateral sclerosis],” the researchers wrote.
“The characterisation of SMA-associated spinal and cerebral pathology and the development of disease-specific biomarkers are particularly timely given the emergence of effective disease-modifying therapies and promising pharmacological trials in SMA,” they added.







