iPSC Technology Spurs Promising Gains in SMA Research
Written by |
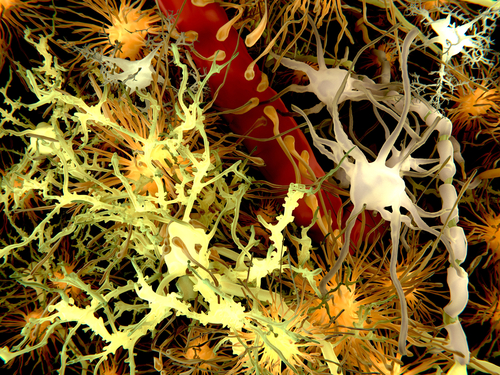
 Spinal muscular atrophy (SMA) is among the many motor neuron diseases that have no cure. One reason for the lack of cures is the inexistence of reliable in vitro disease models to be used as platforms for research and development of new drugs. This is partially attributed to the difficulty in obtaining human neural cells.
Spinal muscular atrophy (SMA) is among the many motor neuron diseases that have no cure. One reason for the lack of cures is the inexistence of reliable in vitro disease models to be used as platforms for research and development of new drugs. This is partially attributed to the difficulty in obtaining human neural cells.
A study from University of Milan in Italy, “Pluripotent Stem Cell-based Models of Spinal Muscular Atrophy,” published in Molecular and Cellular Neuroscience, reviewed one way to mitigate the lack of primary human neural cells for drug discovery. Lead author Dr. Emanuele Frattini and principal investigator Dr. Stefania Corti explained how induced pluripotent stem cells (iPSCs) and human embryonic stem cells (hESCs) can be differentiated reproducibly into neurons and other neuronal subtype cells in the laboratory, but also noted that iPSCs may provide more benefits than hESCs. “Overall, iPSCs appear to have the potential to revolutionize the approach to the study and the treatment of human diseases,” the authors wrote.
Spinal muscular atrophy, which arises from deletions or mutations in the gene encoding survival of motor neuron 1 (SMN1), is the subject of numerous pre-clinical studies involving mice, as the mouse genome is relatively easy to manipulate. Knocking out SMN1 provides an animal model with similar molecular and pathological characteristics of human SMA, but there are still important physiologic and anatomic differences that decrease the validity of the model.
[adrotate group=”3″]
Hence, research has been focused on generating a more reliable model of SMA that involves human cells. iPSCs are used to avoid the lack of primary neuronal cells, as they can be generated from adult human fibroblasts taken from SMA patients and differentiated into neuronal cells to model disease. This was first achieved by a group of researchers at University of Wisconsin-Madison in collaboration with The Waisman Center in 2009. “Induced Pluripotent Stem Cells from a Spinal Muscular Atrophy Patient,” published in Nature, laid the groundwork to derive deficient motor neurons from an SMA patient’s skin fibroblasts. “As such, it represents a promising resource to study disease mechanisms, screen new drug compounds, and develop new therapies,” wrote lead author Dr. Allison D. Ebert and principal investigator Dr. Clive N. Svendsen.
Key findings leading from studies with iPSC-derived SMA-diseased cells involve ways to rescue motor neurons from death. It seems that blocking Fas ligand-mediated apoptosis and altering astrocyte behavior may reduce SMA motor neuron apoptosis. On the treatment front, it has been shown that affecting CD36 may influence valproic acid non-responsiveness in SMA motor neurons and that treating SMA iPSCs with oligonucleotides yields motor neurons adequate for transplantation.
Although many gains have been made using iPSC-derived SMA motor neurons, a long road remains ahead. Scientists continue to work through pre-clinical models and drug discovery tests, but these must be validated in clinical trials before they can be applied to humans with SMA.