Researchers Discover Neural Stem Cells Exert Neuroprotective Effects in SMARD1
Written by |
 A recent study entitled “iPSC-Derived Neural Stem Cells Act via Kinase Inhibition to Exert Neuroprotective Effects in Spinal Muscular Atrophy with Respiratory Distress Type 1” published in Stem Cell Reports suggests therapeutic potential of neural stem cells (NSCs) from human-induced pluripotent stem cells (iPSCs) to ameliorate Spinal muscular atrophy with respiratory distress type 1 (SMARD1).
A recent study entitled “iPSC-Derived Neural Stem Cells Act via Kinase Inhibition to Exert Neuroprotective Effects in Spinal Muscular Atrophy with Respiratory Distress Type 1” published in Stem Cell Reports suggests therapeutic potential of neural stem cells (NSCs) from human-induced pluripotent stem cells (iPSCs) to ameliorate Spinal muscular atrophy with respiratory distress type 1 (SMARD1).
Among genetic disorders, Spinal muscular atrophy (SMA) is the leading cause of death in children. Currently without any FDA-approved treatment, it’s caused by genetic mutation of the Smn1 gene that codes for a protein crucial for motor neurons’ survival. Spinal muscular atrophy with respiratory distress type 1 (SMARD1) is the most frequent form of spinal muscular atrophy after SMA. As with SMA, no therapy is available.
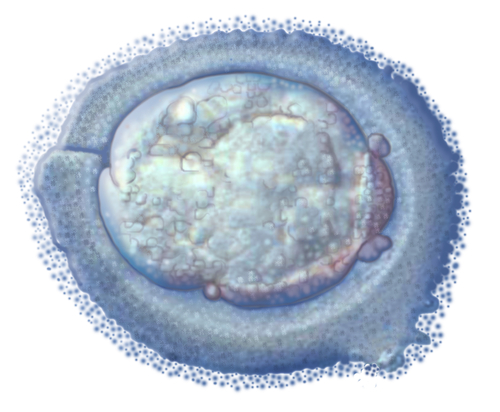
Neural stem cell (NSC) transplantation has been suggested as a therapeutic strategy for neurological diseases, including SMA, SMARD1, and amyotrophic lateral sclerosis (ALS). However, the acquisition of human stem cells is still one of the great limitations for its therapeutic use. Thus, a new technique where somatic human cells can be reprogrammed into induced pluripotent stem cells (iPSCs) can revolutionize the method to acquire these cells, such as NSCs.
In this study, a team of scientists investigated if transplanting human iPSC-derived NSCs into the spinal cord of nmd mice, the animal model of SMARD1, can be used as a therapy. The authors generated and differentiated iPSCs into NSCs. Then, to investigate the therapeutic potential of wild-type (WT) iPSC-derived NSCs, they injected these cells into SMARD1 mice.
[adrotate group=”3″]
At the end stage of the disease, transplanted iPSC-Derived NSCs were found in mice spinal cord. Notably, the transplanted cells could differentiate into the three major neuroectodermal cell lineages. With differentiation, these cells improved motor behavior and extended survival in nmd mice. This was achieved via iPSC-derived NSCs production of the neuro protective factors glial cell-derived neurotrophic factor (GDNF), brain-derived neurotrophic factor (BDNF), transforming growth factor-α (TGF-α), and neurotrophin-3 (NT3). Finally, to understand if their findings translated to humans, the authors reprogrammed fibroblasts and then differentiated them in motor neurons, from both of SMARD1 patients and healthy donors. When human NSCs (hNSCs) were added to SMARD1 motor neurons improved their survival and protected it against degeneration, via inhibition of GSK-3 and HGK kinases.
Thus, the authors suggest NSCs derived from pluripotent cells can be a potential new therapeutic strategy to ameliorate SMARD1 disease phenotype, with possible further positive results if combined with other forms of therapy, e.g. drugs.



