Researchers Targeting Astrocytes Discover Treatment Benefits in SMA-Induced Mice
Written by |
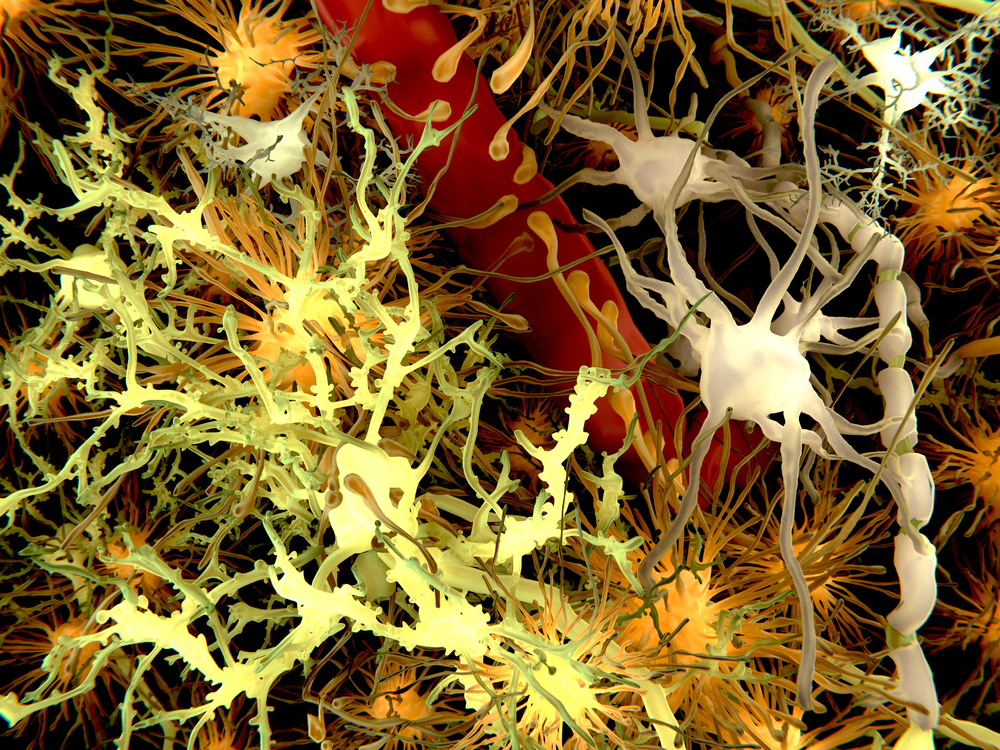
Previously thought to be a disease only of motor neurons, spinal muscular atrophy (SMA) is now also known to be influenced by support cells of the central nervous system. Specifically, astrocytes, which regulate synapse formation between neurons and provide metabolic support for neurons, are essential to the pathogenesis of SMA and are an interesting cell type to direct SMA treatments. A group from the University of Missouri Bond Life Sciences Center and collaborators in UCLA, Johns Hopkins, University of Utah School of Medicine, and Medical College of Wisconsin delved further into the science behind astrocytes in SMA and explored how restoring survival motor neuron-1 (SMN1) in astrocytes benefits mice with severe SMA.
“We hypothesized that astrocyte functions are disrupted in SMA, exacerbating disease progression,” wrote Dr. Hansjörg Rindt, co-lead author with Dr. Zhihua Feng and Chiara Mazzasette, in the article, “Astrocytes Influence the Severity of Spinal Muscular Atrophy,” published in Human Molecular Genetics Advance Access.
To begin the study, the researchers genetically modified astrocytes in mice containing the SMNΔ7 mutation to induce SMN1 expression in astrocytes only. This rescued mice lifespan, doubling the median survival from 16 days to 33 days. The animals also experienced fewer symptoms and increased weight gain, gross motor function, and overall muscle function.
Since SMNΔ7 mice are considered to have the most severe form of SMA, the researchers also wanted to test their genetic modification tools in SMN2B/- mice, whose lifespan is an average of 30-35 days. The genetic alteration in astrocytes increased these animals’ average lifespans to beyond 100 days. The mice also showed normal muscle function and weight.
Part of the reason why the genetic alteration worked is because the altered astrocytes were able to conduct normal functions such as maintain the circuitry between neurons and muscles. While untreated mice had poor innervation of neuromuscular junctions, treated mice had fully innervated neuromuscular junctions.
Adding a human element to these studies, the researchers looked at thin sections of SMA patients’ spinal cords and compared them to sections from non-SMA individuals. Compared to the controls, SMA patients showed increased levels of pro-inflammatory markers produced by astrocytes and other activated glial cells. These results were recapitulated in untreated SMNΔ7 mice, but treated SMNΔ7 mice had lower pro-inflammatory marker levels that were similar to those of normal mice.
“The development of effective therapies for SMA depends on the identification and characterization of pathological changes across tissues and cell types,” wrote the authors. “Although SMA has been widely regarded as a motor neuron-autonomous disorder in the past, a number of recent studies has challenged this view.” This study bolsters the notion that astrocytes are involved in the pathogenesis of SMA and that targeting astrocytes with therapies provides benefits in the case of animal models of the disease.



