SMA Type 3 Adults May Have Issues Regulating Component of Cell’s ‘Skeleton,’ Study Suggests
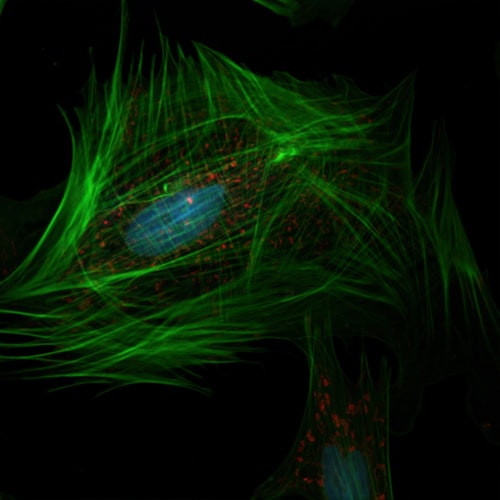
Photo by National Cancer Institute on Unsplash -cytoskeleton
Adults with spinal muscular atrophy (SMA) type 3 have significantly lower levels of several molecules that help regulate actin, one of the major components of the cell’s cytoskeleton, according to a study.
These findings, from blood and connective tissue cells, add to information from a previous study showing impaired actin dynamics in motor neurons from SMA type 1, suggesting that the characteristic loss of SMN protein in SMA patients may affect actin regulation throughout the body.
While larger studies are needed to confirm the results, they may help to better understand the effects of SMN loss in peripheral tissues and provide new therapeutic targets and/or disease biomarkers for adult SMA patients — which are currently lacking, according to the researchers.
The study, “Whole‐blood dysregulation of actin‐cytoskeleton pathway in adult spinal muscular atrophy patients,” was published in the journal Annals of Clinical and Translational Neurology.
Increasing evidence suggests that dysregulation of cytoskeletal proteins contributes to neuron loss in neurodegenerative diseases, including amyotrophic lateral sclerosis, Alzheimer’s disease, Parkinson’s disease, Charcot-Marie Tooth, and Friedreich’s ataxia.
The cytoskeleton is a network of filaments or fibers (including actin) that regulates the cell’s shape and movement, as well as the transport of molecules within the cell.
Notably, defects in actin dynamics were reported in motor neurons of patients with SMA type 1 and in yeast and other models of SMA, a neurodegenerative disease caused by low SMN levels. Deficient levels of SMN, a protein produced throughout the body and key for the health of muscle and motor neurons, leads to the loss of motor neurons, resulting in muscle weakness and wasting.
“However, little is known about how the actin cytoskeleton is regulated in cells or tissues in SMA patients,” the researchers wrote.
In addition, there is limited data on protein level changes in adults with SMA, challenging the identification of potential therapeutic targets or biomarkers in this subgroup of patients.
Aiming at identifying potential therapeutic targets for SMA adult patients, researchers at the Massachusetts General Hospital’s Center for Genomic Medicine and the Broad Institute of MIT and Harvard discovered that actin regulation is also impaired in adults with the milder type 3 disease.
They searched for significant changes in the activity of more than 10,000 genes in blood samples of 31 adults with SMA type 3, compared with those of 34 age- and gender-matched healthy individuals, used as controls.
Results showed that 287 genes were significantly more active and 270 significantly less active in SMA patients than in healthy people. Pathway analysis identified three signaling pathways significantly boosted and seven significantly suppressed in adults with SMA, compared with controls.
Regulation of actin cytoskeleton was the most suppressed pathway in SMA patients and was therefore selected for further analyses.
When looking at the blood levels of molecules involved in that pathway the team found that type 3 patients had a 43% decrease in the levels of beta-actin, a type of actin, and about a 20% drop in the levels of two actin regulators of the Rho GTPase family (RHOA and ROCK1), compared with healthy people.
This significant reduction in the levels of beta-actin and actin regulators in adults with SMA was also confirmed in fibroblasts (cells of the connective tissue) collected from patients.
Notably, promoting the production of high SMN levels in patients’ fibroblasts failed to restore the levels of actin-associated proteins, suggesting that “changes in the [levels] of key regulators of actin cytoskeleton are not directly associated with acutely reduced SMN levels,” the researchers wrote.
They hypothesized that “changes in the regulation of actin cytoskeleton are therefore consequences of chronic low SMN levels” and increasing SMN levels is not “sufficient to induce all adaptations necessary to reestablish the regulation of actin cytoskeleton.”
These findings implicate, for the first time, altered actin cytoskeleton dynamics in peripheral cells and tissues in adult SMA patients, contributing to the understanding of SMN deficiency effects in several tissues of these older patients.
The results suggest that the actin regulation pathway may include potential therapeutic targets and/or biomarkers for people with SMA, including adults, according to the team.
They also emphasized that further studies with larger groups of participants are needed to confirm these findings and to evaluate other pathways found to be significantly suppressed in this study, such as those involved in immune responses and mitochondria metabolism.







