Using Ultrasound May Help in SBMA Diagnosis, Study Shows
Written by |
Men with spinal and bulbar muscular atrophy (SBMA) were found to have abnormally small nerves in the limbs, especially the arms, as measured by ultrasound, a study showed.
These findings support the use of ultrasound as an additional tool to identify SBMA and improve selection for genetic testing, the scientists said.
“In this small study of SBMA patients, the ultrasound changes were striking and sufficiently severe to be detected in individual patients,” the researchers wrote.
The study, “Nerve ultrasound detects abnormally small nerves in patients with Spinal and Bulbar Muscular Atrophy,” by researchers based at Tauranga Hospital, in New Zealand, was published in the journal Muscle & Nerve.
SBMA, also referred to as Kennedy’s disease, is an adult-onset form of spinal muscular atrophy that mainly affects men and progresses very slowly.
The condition is caused by inherited defects in the androgen receptor gene, which encodes for a protein that binds androgens — a group of hormones that includes testosterone — that are important for male development. However, how androgen receptor defects lead to damage in nerves that control movement, or motor neurons, remains poorly understood.
Hallmarks of SBMA are progressive weakness and atrophy (shrinkage) in the muscles closer to the body, such as the arms and legs, and the bulbar muscles of the mouth and throat.
Nerve abnormalities in SBMA have been observed beyond motor neurons, including in the dorsal root sensory ganglia — a group of nerve cells adjacent to the spinal cord that relay sensory information, such as touch or heat, from the extremities to the spinal cord and brain.
In some cases, however, sensory nerve impairment may go undetected as symptoms are subtle. Moreover, findings from nerve tests may not meet the diagnostic criteria for sensory-related nerve damage (sensory neuropathy), leading to missed or delayed diagnoses.
Ultrasound has been used to identify smaller nerves that result from other conditions associated with sensory neuropathy, but not in patients with SBMA.
“We investigated the hypothesis that patients with SBMA show the reduction in nerve size characteristic of other inherited sensory neuronopathies, suggesting a role for ultrasound in the evaluation of patients with possible SBMA,” the researchers wrote.
The team recruited seven men with genetically confirmed SBMA without a history of neuropathy, diabetes, or other conditions associated with nerve damage. A group of 18 patients with acquired sensory neuropathy, the majority caused by diabetes, was included as a comparison alongside 42 neurologically healthy people as a control group.
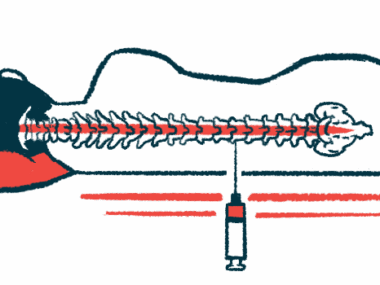
Ultrasound was used to measure the cross-sectional area of the median and ulnar nerves that extend through the arm and the sural nerve of the calf, and the tibial nerve behind the knee joint. All patients underwent electrical conduction tests (electrophysiology) of motor and sensory nerves in similar areas.
The analysis revealed that the cross-sectional areas of nerves in SBMA patients were significantly smaller than those of the neuropathy patients and the controls at all sites measured.
Differences were more pronounced in the upper limbs, with mean upper limb cross-sectional areas in SBMA patients one-third smaller than acquired neuropathy patients and about half the size of healthy controls. On average, the upper limb nerves in acquired neuropathy patients were more than a quarter larger than controls.
When compared with reference values, the individual upper limb nerve cross-sectional areas were smaller in all SBMA patients, compared with none in the acquired neuropathy patients.
Sensory nerve conduction tests showed reduced electrical signals in six SBMA patients. Signals generated due to muscle contractions were lower in the median and/or ulnar arm nerves in all seven SBMA patients and the tibial and/or peroneal nerve just below the knee in two.
Acquired neuropathy patients also had reduced or absent nerve signals and normal or slightly reduced signal speeds. Muscle contraction signals were lower in the tibial and/or peroneal nerve in 12 of these patients.
While the study was small, the researchers noted that the changes shown via ultrasound were “striking ” and severe enough to be detected in individual patients.
“This suggests that ultrasound could be used as an additional tool for the identification of SBMA in patients with lower motor syndromes, which could also improve efficiency for selection of genetic testing,” the team wrote.
“Future studies on a larger population are planned to confirm these preliminary findings, explore correlations between ultrasound, electrophysiology, [genetic defects] and clinical parameters of disability, and establish the stage in the disease course when the ultrasound abnormality becomes evident,” they added.