Lack of Muscle Cell Signaling Seen to Kill Motor Neurons in SMA-LED2
Written by |
Problems with the secretion of survival signals from muscle cells seems to be the dominant driver of motor neuron loss in spinal muscular atrophy lower extremity predominant 2 (SMA-LED2), an SMA subtype largely affecting the legs, a study suggests.
The study, “Loss of BICD2 in muscle drives motor neuron loss in a developmental form of spinal muscular atrophy,” was published in Acta Neuropathologica Communications.
SMA-LED is characterized by the death of motor neurons (the nerve cells that control movement), particularly affecting the lower limbs. It is caused by mutations in one of two genes, DYNC1H1 or BICD2, which encode proteins of the same names.
SMA-LED type 1 or SMA-LED1 is marked by mutations in the DYNC1H1 gene, and SMA-LED type 2 or SMA-LED2 by mutations in the BICD2 gene.
Although several studies have been preformed in different animal models, the exact mechanisms that connect these mutations to motor neuron death is still a matter of investigation.
Researchers worked with mice that had been engineered to completely lack BICD2. According to their study, these mice “show similar clinical features” to humans with “severe” BICD2 mutations, such as the accumulation of fluid in the brain (hydrocephalus).
The researchers examined nerves toward the base of the mice’s spinal cords, and found selective death of motor neurons. That is, motor neurons — specifically, motor neurons with a diameter between 2.5 and 4 μm — died, but other types of neurons (i.e., sensory neurons) did not die.
This could be caused in one of two ways: either the lack of BICD2 resulted in problems in the motor neurons themselves, causing their death (called an autonomous mechanism). Or it caused problems elsewhere in the body, affecting only motor neurons as a downstream consequence (referred to as a non-autonomous mechanism).
To find out which was the case, the researchers generated mice that lacked BICD2 in only motor neurons. However, these mice didn’t have significantly fewer motor neurons compared to wild-type (healthy) mice.
They then generated mice that lacked BICD2 specifically in muscle cells. In these mice, significant motor neuron loss occurred, comparable to what was seen when BICD2 was lacking in all cells. This suggested that the lack of functional BICD2 in muscle cells is the primary driver of motor neuron cell death.
“We have shown that loss of BICD2 leads to death of motor neurons and that this is a non-cell autonomous process driven by the loss of BICD2 in muscle,” the researchers wrote.
They offered an explanation for this phenomenon based on the neurotrophin hypothesis, a model of motor neuron development.
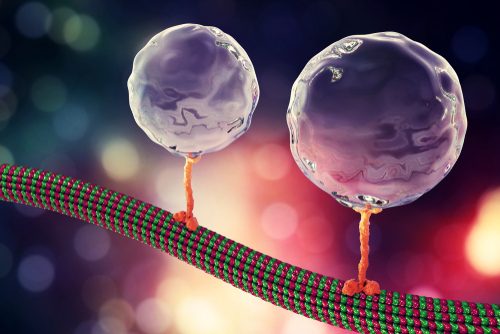
Simply put, this model suggests that, early on in development, an abundance of motor neurons all connect to the same muscle cells. Then, muscle cells secrete molecules that signal the motor neurons to survive (neurotrophins), but the excess motor neurons don’t get these signals and die off. Conceptually, this process results in a ‘just right’ number of motor neurons for each muscle fiber.
The researchers noted that both BICD2 and DYNC1H1 have been implicated in cell secretory pathways. They suggested that the underlying problem in the muscle cells could be problems in cell secretion, which would result in fewer survival signals being sent to motor neurons.
In preliminary support of this idea, skin cells taken from three people with SMA-LED2 were examined and compared to cells from three people without SMA-LED2 of a similar age as a controls. The SMA-LED cells showed secretion deficits, with slower secretion than the control cells.
“How such a delay in secretion causes a significant loss of motor function can be explained in light of the neurotrophin hypothesis,” the researchers wrote. “In this model, a reduction in the rate of secretion would yield a decrease in neurotrophin availability, driving an excess of motor neuron death.”
Although they only directly examined mutations in BICD2, the researchers wrote that this model, “is also likely to be applicable to SMALED caused by mutations in DYNC1H1.”
The researchers noted that this model contradicts findings of previous work in flies, which suggested that motor neuron defects were a direct result of a lack of BICD2 in the motor neurons themselves — that is, an autonomous mechanism.
They speculated that this contradiction might be attributable to differences between the species studied, writing that flies, “display important differences to mammals in the neurotrophin pathway [at the juncture of motor neurons and muscle cells].”
Further research will be needed to fully understand the reasons for these disparate findings, and to more fully understand what specific signals from muscle cells are being disrupted.
“However,” the researchers wrote, “the most important point to clarify in future studies is likely to be the precise time point at which motor neuron loss occurs, which is important when considering future therapeutic interventions in SMALED2 patients.”