Measuring Neurological Impact of Polio Proves Useful in SMA, Study Reports
Andrii Vodolazhskyi/Shutterstock
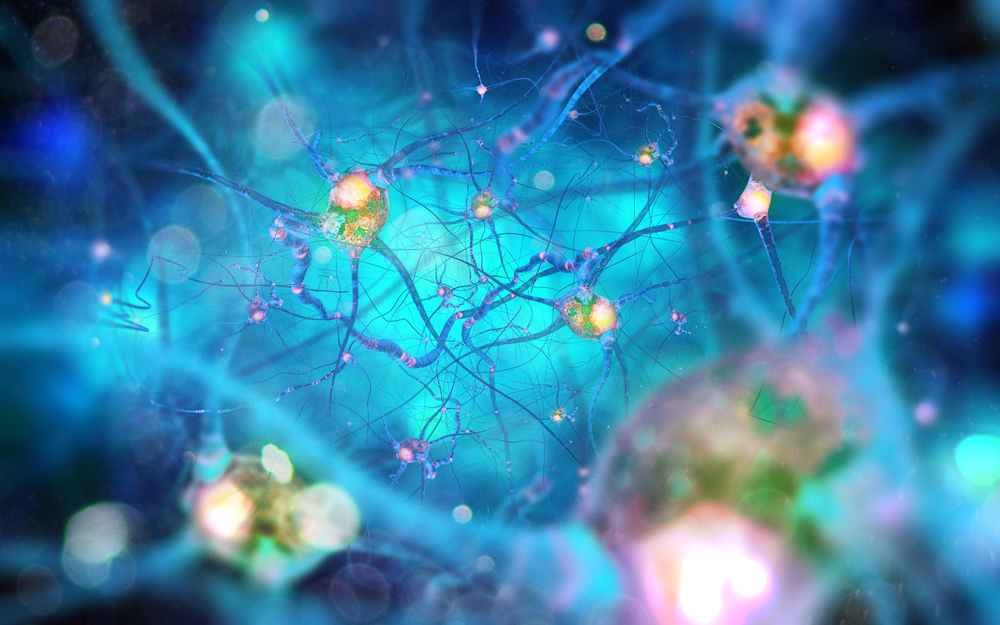
Researchers have found changes in the electrical activity between the brain and muscles in adults who had childhood polio — an infection that affects the same motor neurons as those impacted in people with spinal muscular atrophy (SMA), a study reported.
The inexpensive and non-invasive technique used to measure these changes can also be employed to find the neurological networks responsible for daily movements in SMA, the researchers said. Moreover, the technique can further be used as a biomarker to assess the impact of disease-modifying therapies.
The study, “Altered supraspinal motor networks in survivors of poliomyelitis: A cortico-muscular coherence study,” was published in the journal Clinical Neurophysiology.
The poliovirus can cause paralysis by attacking motor neurons in the spinal cord and the brain; the same nerve cells are affected in people with SMA.
Recent imaging studies have found similar alternations in the connections of nerve fibers in people with polio and SMA.
Thus, understanding these changes in adults who had polio as children may provide insight into SMA. It also could impact patient treatment as well as the discovery and testing of potential new therapies.
Now, researchers based at Trinity College Dublin, in Ireland, designed a study to investigate alterations in polio survivors’ motor networks by measuring brain activity using electroencephalogram (EEG), a test that detects abnormalities in brain electrical activity, and assessing muscle activity by electromyography (EMG), which measures electrical muscle activity in response to muscle nerve stimulation.
The team used an approach known as cortico-muscular coherence (CMC), which measures the synchronized coordination (coherence) between motor brain activity and associated muscle activity.
The study included 24 people — 17 women and seven men, with a current mean age of about 67 — who had polio in childhood, along with 11 age-matched healthy individuals (controls). Among the polio survivors, eight contracted polio in the first two years of life while 16 were infected after age 2.
EEG, done on the scalp, and EMG, measured on the wrist, were recorded during a pincer grip task, in which the thumb and the index finger of the right hand were squeezed together on a sensor guided by visual cues. The CMC was calculated between the EMG signals from the hand muscles and the EEG.
Differences in the CMC were identified between former polio patients and the healthy controls. Specifically, in the patient group, the CMC pattern did not show a beta band brain wave pattern (14 to 30 Hz) commonly seen in sustained weak muscle contractions in the healthy controls. The CMC also was scattered and inconsistent across five tested EEG electrodes, three muscles, and frequency bands.
Of note, brainwaves are produced by electrical pulses from nerve cells (neurons) communicating with each other. They are divided into different bandwidths, specifically infra-low, delta, theta, alpha, beta, and gamma, that change according to what an individual is doing and feeling.
Overall, the difference in the CMC in patients versus controls was statistically significant. The polio survivors’ CMC frequencies were consistently found in the low gamma (31 to 47 Hz) frequency band across several EEG-EMG channels, which are associated with more strong muscle contractions.
Importantly, this abnormal low gamma-band coherence was observed not only over the primary motor areas of the brain but also over the frontal lobe and parietal lobe, or midbrain areas.
Thus, these CMC patterns differed from the control group in both frequencies (beta vs. low-gamma) and brain location.
“These findings imply a differential engagement of cortical networks in polio survivors that extends beyond the motor cortex and suggest a disease-related functional reorganisation of the cortical motor network,” the researchers wrote.
The Trinity investigators said studying these polio survivors can help scientists today in building treatments for now-common conditions like SMA and amyotrophic lateral sclerosis (ALS). Findings from such studies could impact rehabilitation for SMA and ALS patients, aid in the discovery of effective medications, and help quantify the potential effectiveness of new treatments.
“Our research findings show for the first time that the brain ‘rewires’ in those who suffered from polio in childhood,” Orla Hardiman, MD, a study co-author, said in a press release.
“This has implications for our understanding of brain plasticity,” Hardiman added. Of note, brain plasticity refers to the ability of synapses, the junctions between two nerve cells that allow them to communicate, to strengthen or weaken over time.
A comparison of polio survivors who contracted the disease before age 2 with those infected after that age also found differences in CMC, which likely reflects differences in compensatory patterns that occur as nerves mature, the researchers noted.
These results have implications for SMA as well, in which “a consistent abnormal CMC measure in (adult) SMA, could be used as a potential biomarker to track network function,” the researchers wrote.
“Such biomarkers can identify network-level changes associated with lower motor neurons following administration of a disease-modifying agent, thus providing a quantitative biomarker of efficacy in clinical trials,” they wrote.
“This study is especially interesting because it shows that advanced methods in neurophysiology and neural signal analysis can help to unravel new aspects of how different diseases disrupt our movements,” said Bahman Nasseroleslami, PhD, assistant professor, clinical medicine, at Trinity and a study senior author.
“These types of inexpensive non-invasive methods can be further developed for probing the different “neural networks” in humans that are responsible for different day-to-day movements and different diseases that affect them,” Nasseroleslami said.
Amina Coffey, PhD, the study’s first author, added, “This study shows that neurophysiological markers can pick up changes in brain connectivity patterns that have implications in our understanding of other similar neurological conditions like Spinal Muscular Atrophy.”