Motor unit changes track with SMA severity, new study shows
Nerve-muscle signal patterns may help doctors better assess SMA progression
Written by |
- People with more severe SMA had fewer motor units, and the remaining ones were unusually large.
- These nerve–muscle changes were strongly linked with current motor ability.
- Researchers say these measures may help doctors better assess SMA severity and treatment effects.
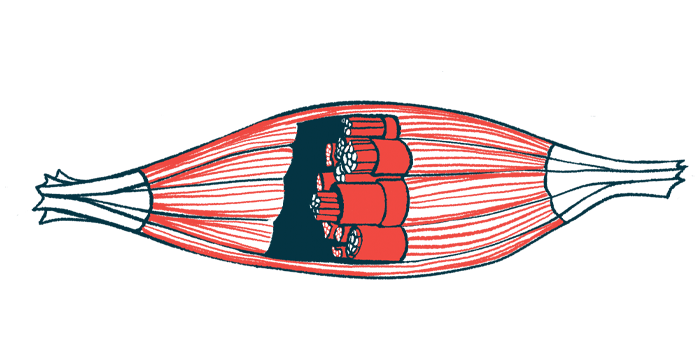
Changes in the motor unit, which is made up of a nerve cell and the muscle fibers it controls, may help doctors better understand how severe spinal muscular atrophy (SMA) is in each person, according to a new study.
The researchers found that people with more severe SMA had fewer motor units, which likely reflects a greater loss of the nerve cells that control movement (motor neurons). The motor neurons that remain often “take over” extra muscle fibers, leading to unusually large motor units. These changes were seen even in some people whose overall muscle response still appeared normal on routine testing.
Problems in nerve-muscle communication at the neuromuscular junction (NMJ), where nerves connect to muscles, were also more common in people with greater motor disability.
“These measures may serve as complementary biomarkers for disease severity in patients with SMA,” the researchers wrote.
The study, “Motor Unit Patterns Correlate With Severity in Symptomatic Patients With Spinal Muscular Atrophy,” was published in the European Journal of Neurology.
Motor neuron loss drives muscle weakness in SMA
SMA is caused by the gradual loss of motor neurons. As more of these cells are lost over time, muscles become weaker and smaller, leading to hallmark SMA symptoms and a gradual loss of movement abilities.
The severity and age at which symptoms begin vary by SMA type. The most severe is SMA type 0, which appears before or at birth, while SMA type 4 is the mildest and usually begins in adulthood.
Newer disease-modifying treatments have changed the outlook for people with SMA. However, outcomes depend greatly on how advanced the disease is when treatment begins. Starting therapy earlier — even before symptoms appear — is associated with more favorable results.
Doctors usually measure disease severity and progression using functional motor scales, standardized tests that rate a person’s ability to perform movement-related tasks. But these tests may not detect small changes over short periods of time, and they cannot be used to define disease severity before symptoms begin.
“We therefore need to develop more sensitive methods to predict and determine disease stage, and effectively monitor disease progression and treatment effects,” the researchers wrote.
Because motor unit changes may reflect what is happening biologically in SMA, researchers in the Netherlands set out to test whether these changes could be used as biomarkers — measurable signals — of disease severity and progression across the full range of SMA types.
Researchers analyze motor unit changes across the SMA spectrum
The study took place at the Netherlands SMA Centre at the University Medical Centre Utrecht. It included 104 adolescents and adults with symptomatic SMA types 1 through 4 who had not yet started disease-modifying treatment. The study period ran from May 2020 through July 2022. Another 65 healthy people were included as a comparison group (controls).
The median age of people with SMA was 39 years, compared with 58 years in the control group. The median when symptoms first began ranged from about 6 months in SMA type 1 to around 2 years in SMA types 3 and 4. Median disease duration ranged from about 29 years in SMA type 2 to around 44 years in SMA types 3 and 4.
Using noninvasive electrical testing of nerves and muscles, the researchers found clear signs that motor units were altered in people with SMA. Compared with healthy controls, people with SMA had significantly fewer motor units overall. The remaining motor units were often larger than normal, likely because surviving motor neurons had taken over extra muscle fibers.
Even though only 38% of participants had a reduced overall muscle response, and 7% had severely reduced responses, most people (83%) who still showed normal overall muscle responses already had signs of motor unit loss or enlargement.
We identified altered motor unit patterns and NMJ function in patients with SMA, with distinct patterns across SMA severity independent of age or disease duration.
Motor unit patterns also varied by disease severity. People with the greatest disability, such as those unable to sit independently, showed severe loss of motor units, with only a few enlarged units providing most of the muscle’s electrical signal. By contrast, people who were still able to walk generally retained more motor units, with less dominance of enlarged units.
Importantly, these motor unit patterns were strongly linked to current movement ability but were not related to age or how long a person had been living with SMA.
Signs of NMJ dysfunction, problems in how nerves and muscles communicate, were also common across SMA types. About 13% of people showed a 10% or greater drop in muscle response during repeated nerve stimulation. A milder drop of at least 5% occurred in 38% of participants and was seen more often in people with more severe movement problems.
People with NMJ dysfunction also tended to have fewer motor units overall, with a larger share of the muscle signal coming from the enlarged motor units.
Nerve–muscle signal changes mirror real-world motor ability
The electrical measurements from nerves and muscles closely matched how well people functioned in daily life. People who scored higher on functional motor tests generally had more preserved motor units and less reliance on abnormally enlarged units. Those with lower motor scores tended to have greater motor-unit loss, with most muscle activity coming from a smaller number of enlarged units.
“These findings further emphasize that the observed motor unit patterns are linked to motor function in patients with SMA,” the researchers wrote.
“We identified altered motor unit patterns and NMJ function in patients with SMA, with distinct patterns across SMA severity independent of age or disease duration,” the scientists concluded, noting that “these measures may serve as complementary biomarkers for disease severity in patients with SMA.”
They also wrote that future studies should examine “whether [these] motor unit pool patterns are present in early and even presymptomatic stages of the disease and validate their value as biomarkers for treatment efficacy.”