New patient-derived cell models may advance SMA, SMARD1 study
Approach can be used to explore patient-specific mechanisms, therapy response
Written by |
Researchers have developed new patient-derived cell models of spinal muscular atrophy (SMA) caused by SMN1 mutations as well as the more rare spinal muscular atrophy with respiratory distress type 1 (SMARD1).
The cells exhibited structural abnormalities consistent with SMA which could be rescued with gene therapies.
Scientists believe the new in vitro — or in-the-lab — approach can be used to explore patient-specific disease mechanisms, including for patients who have genetic mutations with an unknown significance, and to probe their potential responsiveness to therapies.
“These findings could help improve our understanding of SMA and SMARD1/CMT2S, as well as aid in the development of new treatments for these diseases,” researchers wrote.
The study, “In Vitro Modeling as a Tool for Testing Therapeutics for Spinal Muscular Atrophy and IGHMBP2-Related Disorders,” was published in Biology.
No DMTs available for SMARD1, an extremely rare disease type
The most common forms of SMA are caused by mutations in the SMN1 gene, leading to symptoms of muscle weakness and wasting due to a lack of the SMN1 protein. Three disease-modifying treatments are currently approved for these forms of SMA, including Evrysdi (risdiplam), Spinraza (nusinersen), and Zolgensma, a gene therapy.
On the other hand, SMARD1 is an extremely rare type of SMA caused by mutations in IGHMBP2, a gene with a poorly understood function, and for which there are no disease-modifying treatments available.
IGHMBP2 variants can lead to a wide spectrum of symptoms, ranging from severe muscle weakness and respiratory failure in SMARD1, to more mild neuromuscular diseases without respiratory involvement, such as Charcot-Marie-Tooth disease type 2S (CMT2S).
Currently, no approved therapies specifically target IGHMBP2, but the researchers previously developed a gene therapy that is currently in a Phase 1/2a clinical trial (NCT05152823) for IGHMBP2-related disorders at Nationwide Children’s Hospital in Ohio.
Similarly to Zolgensma, which provides patients with a healthy version of SMN1, the experimental gene therapy, called AAV9.IGHMBP2, is designed to provide patients with a working copy of IGHMBP2.
These findings could help improve our understanding of SMA and SMARD1/CMT2S, as well as aid in the development of new treatments for these diseases.
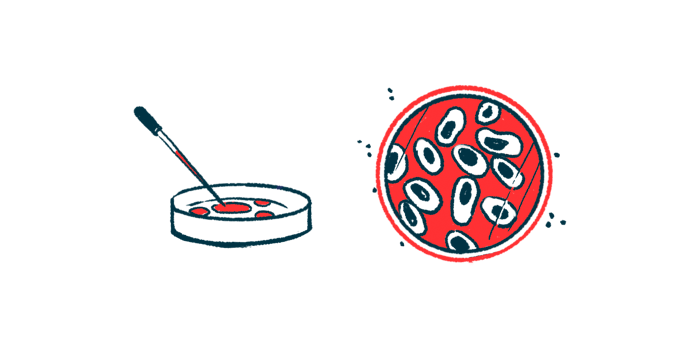
Scientists used patient-derived fibroblasts and converted them into nerve cells
In the study, the researchers generated new nerve cell models of SMA and SMARD1/CMT2S, using them to study disease characteristics and responses to gene therapy.
Their approach involved taking fibroblasts — a type of connective tissue cell with the capacity to differentiate into other cell types — directly from patients’ skin and converting them into nerve cells using various chemicals.
Nerve cells derived from SMA patients with SMN1 mutations exhibited a number of structural changes relative to cells derived from healthy people, including shorter nerve cell projections (neurites) and reductions in SMN protein levels.
Administration of Zolgensma to the cells significantly reversed these deficits and restored more normal SMN levels.
Next, the team generated a similar nerve cell model using fibroblasts taken from two SMARD1/CMT2S patients with IGHMBP2 mutations who were in the middle of the disease spectrum.
Nerve cells derived from these patients also exhibited structural changes relative to healthy cells, including fewer and shorter neurites. More normal structure was restored upon treatment with AAV9.IGHMBP2.
Model could be used to study effects of mutations with unknown significance
The scientists emphasized that their pipeline for generating nerve cells from patient fibroblasts can also be used to study the effects of genetic mutations with an unknown significance.
As an example, the team obtained fibroblasts from a person who had suspected SMARD1/CMT2S. The individual had a known disease-causing mutation in one copy of their IGHMBP2 gene, and another mutation whose significance could not be determined in bioinformatic analyses.
Examining nerve cells derived from that patient, the researchers found that the cells had altered characteristics similar to their previous observations in SMARD1/CMT2S patient-derived cells, including shorter and fewer neurites, which could be rescued with AAV9.IGHMBP2.
According to the scientists, those results suggest that the variant of unknown significance was likely disease-causing.
Overall, the scientists believe that their method for converting patient cells into nerve cells offers several advantages over other approaches, including a faster process and the ability to retain certain cellular characteristics that could influence disease severity.
“We are excited to continue exploring the potential applications of these cells in future studies,” the team concluded.