Why SMN Deficiency So Quickly Kills Motor Neurons Detailed in Study with Relevance to SMA Treatment
Written by |
Researchers may finally have figured out why a loss in the SMN protein that is crucial for all cells so quickly affects motor neurons, leading infants to develop spinal muscular atrophy (SMA).
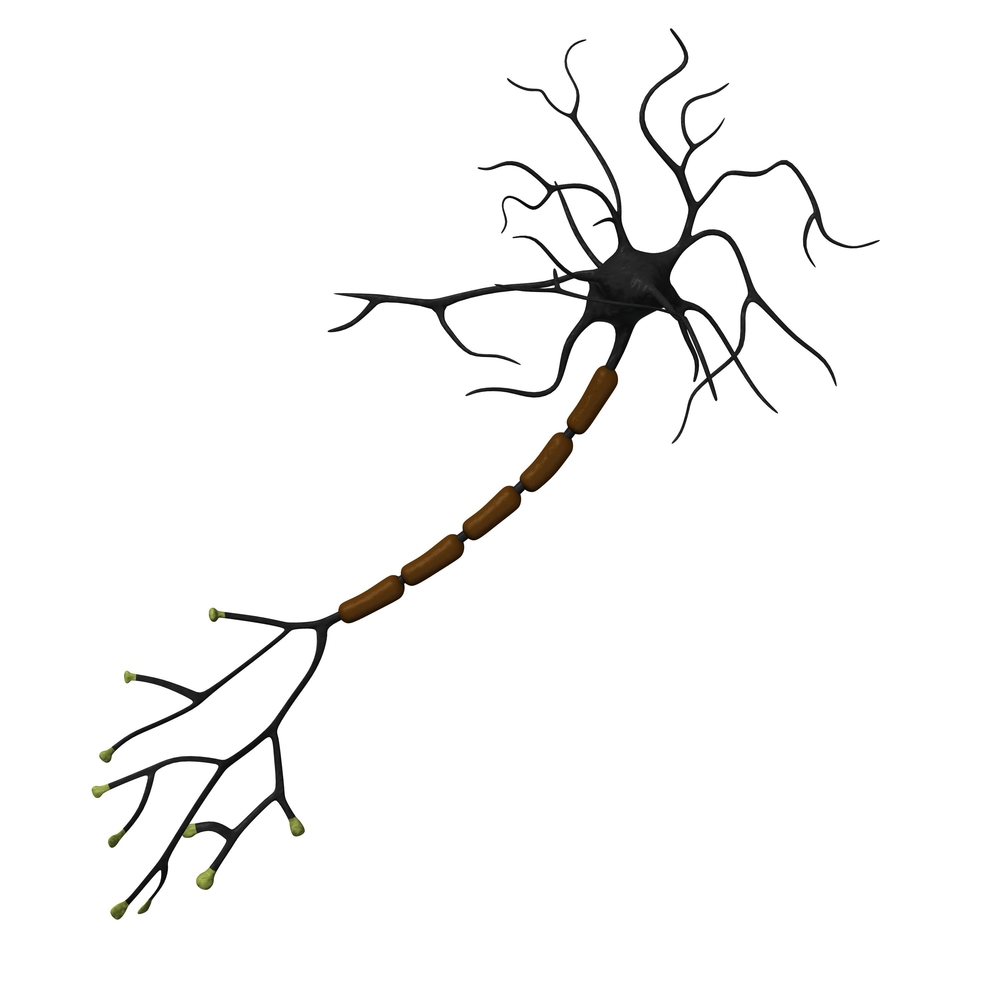
SMN aids in the transport of certain molecules in all cells, processing RNA, and the mutation-caused drop in its levels within cells affects that transport. Since spinal motor neurons have particularly long axons — cell extensions sending signals to other cells — RNA is unable to reach the tip of these axons, causing the neurons to rapidly die, the scientists reported.
Findings in the study, “The Survival of Motor Neuron Protein Acts as a Molecular Chaperone for mRNP Assembly,” published in the journal Cell Reports, may also help to make a newly approved treatment for SMA more effective.
“Our model explains the specificity — why motor neurons are so vulnerable to reductions in SMN,” Wilfried Rossoll, PhD, an assistant professor of cell biology at Emory University School of Medicine and the study’s senior author, said in a press release. “What’s new is that we have a mechanism.”
In a healthy cell, messenger RNA molecules, transcribed from DNA molecules, are released from the nucleus to be used as blueprints for protein production. But they cannot get to their cellular destination on their own, and complex machinery exists to make sure they end up in the right place for proteins to be formed.
According to the Emory research team, the SMN protein, previously suggested to be involved in RNA processing, is part of this machinery. Each RNA has a “zip code” region, telling the machinery precisely where it must go. SMN makes sure the zip code region and the transport protein are in communication.
“It loads the truck, but it’s not on the truck,” said Rossoll. Scientists call this type of molecule a “molecular chaperone.”
The discovery was achieved using a combination of advanced imaging, visualizing cell processes, and biochemical methods. It opens the way for further research into processes that may eventually lead to specific treatments.
Researchers also suggest that their work may help to optimize the delivery of Spinraza (nusinersen), the first approved therapy for SMA. Spinraza increases the amount of functional SMN produced by the SMN2 gene (people have two of these genes), and if the resulting protein could be delivered to neurons in a more targeted and effective manner, the treatment’s benefits might be amplified.



