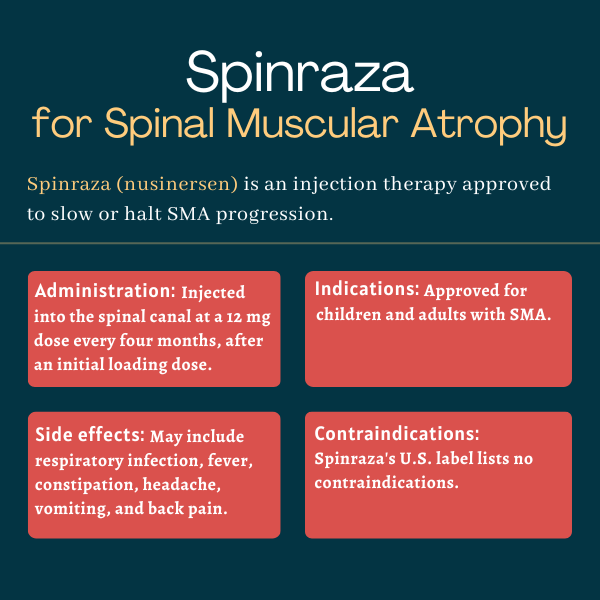
FAQs about Spinraza
The U.S. Food and Drug Administration (FDA) approved Spinraza for the treatment of spinal muscular atrophy (SMA) in 2016. This was a landmark approval, as no other disease-modifying therapies that could target the underlying cause of SMA had been approved at the time.
Spinal muscular atrophy (SMA) is a progressive disease that manifests differently patient to patient, and responses to treatment also will vary. Still, in a Phase 3 trial that tested the therapy in individuals with type 1 SMA, a severe form of the disease, about 41% of patients had attained new motor milestones after six months of treatment, which was not observed in any of the control patients.
Based on clinical trial data, the most common side effects of Spinraza include respiratory infection, constipation, fever, headache, vomiting, and back pain. Another adverse event that has been reported more commonly in Spinraza-treated patients than in controls is post-lumbar puncture syndrome, a complication of the injection characterized by a headache that typically starts from several hours up to two days after the procedure, and which may be accompanied by vomiting, nausea, and dizziness.
According to Spinraza’s U.S. label, the medication may cause a reduction in growth, namely in height, when given to infants. Because Spinraza can cause blood clotting abnormalities, patients also may be at a greater risk of developing bleeding complications and should be monitored regularly. It is recommended that patients, or families of patients, planning to initiate treatment with Spinraza talk with their healthcare team to know more about the potential complications of this treatment and how to prevent or minimize them.
Yes, Spinraza is now approved for both children and adults with spinal muscular atrophy in more than 50 countries. While the medication has mostly been tested in children with the disorder, clinical data have shown Spinraza also can improve or stabilize motor function in adults with milder forms of the disease.
Related Articles

 Fact-checked by
Fact-checked by