Unusual SMN1 mutations detected with ultra-long DNA sequencing
Study underscores importance of ultra-LRS in clinical application of the disease

Unusual mutations in the SMN1 gene, the underlying cause of spinal muscular atrophy (SMA), were detected in two young patients using ultra-long read sequencing (ultra-LRS), a method to analyze large segments of DNA.
“Our study highlights the importance of ultra-LRS in the clinical application of SMA,” the researchers noted in “Novel Alu-mediated deletions of the SMN1 gene were identified by ultra-long read sequencing technology in patients with spinal muscular atrophy,” which was published in Neuromuscular Disorders.
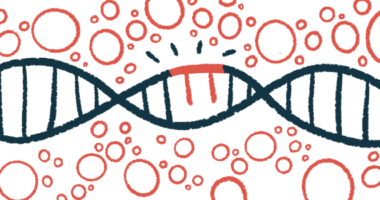
The most common cause of SMA — accounting for about 95% of cases — is the complete loss of exon 7 in both copies of the SMN1 gene, one from each parent. Exons are the sections of a gene that contain information to make proteins. They are interspersed between other regions of the genetic code called introns, which are removed before protein production.
Such double exon deletions result in a deficiency in SMN, a protein essential for the function of nerves that connect with muscles. Low levels of SMN trigger symptoms such as muscle weakness and wasting. Disease severity is largely dictated by the number of the “backup” SMN2 gene, which also produces some SMN protein.
Researchers in China described the cases of two people diagnosed with SMA who carried unusual SMN1 mutations.
Two patients with unusual SMN1 gene mutations
SMA was suspected in one patient after his motor abilities regressed at 11 months of age, which prompted a hospital visit at age 3. The patient was diagnosed with SMA type 2, based on a physical examination, muscle biopsies, and the presence of scoliosis, a sideways curvature of the spine.
The patient was treated with the approved SMA therapy Spinraza (nusinersen), which improved motor function. A genetic analysis to confirm the diagnosis failed to identify a clear genetic cause, however, leading the researchers to apply ultra-LRS to samples collected from the patient and his parents.
Ultra-LRS detected a deletion in the SMN1 gene from the mother encompassing the initial region of the gene, exon 1, and part of the following intron, called intron 1. A hybrid gene from the father was also found, formed by exons 1 through 7 of the SMN2 gene and exon 8 of SMN1.
While hybrid SMN genes have been found in unaffected people, “this is the first reported case of SMA with a partial deletion of SMN1 combined with a hybrid SMN gene,” the researchers noted.
Further analysis showed significantly lower SMN1 gene activity in the patient’s cells, but not in his parents. Consistently, SMN protein levels were reduced compared with an unaffected control with two SMN1 and two SMN2 genes, but higher than a SMA type 1 patient with no functional SMN1 genes and two SMN2 genes.
“This may be due to the fact that [the patient] carried zero copies of SMN1 and two SMN2 and one copy of the hybrid SMN gene,” the researchers wrote, and “may be equivalent to three SMN2 copies,” thus explaining the SMA type 2 diagnosis, which is less severe than type 1.
The second patient was also suspected of SMA but died of severe pneumonia, lung failure, and muscle weakness at 2 months of age. Initial genetic testing revealed a deletion in only one of the SMN1 copies.
Due to the patient’s death, ultra-LRS was performed on his father. Results revealed he also carried a similar but larger mutation, like the first patient, in the exon 1 to intron 1 regions of the SMN1 gene. Researchers suggested his mother had a complete deletion of one SMN1 gene, which her son inherited, explaining the SMA type 1 diagnosis.
Ultra-LRS was applied to find the SMN1 gene deletion breakpoints, the precise location within the gene where the deletion occurred in both patients.
Breakpoint ends were found within the Alu-repetitive elements, types of transposable elements, which are gene segments that readily change positions within DNA, causing deletions. Alu-repetitive elements account for 11% of the human genome, the collection of all genes in a cell.
“Our study indicates that Alu-mediated rearrangements are a mechanism for the evolution of these deletions,” the researchers wrote, adding given the high number of Alu elements in the introns of both SMN genes, “we would expect deletions or duplications caused by Alu elements might not be rare in SMA.”
“We used ultra-LRS to identify and unveil the molecular mechanisms of SV [structural variations] involved in the SMA,” they said. “Our study suggests Alu-mediated SV may be more common than previously anticipated in patients with SMA. These findings expand our perspective on the understanding and considerations of diseases in clinical practice.”