3-D Cell Model Mimics SMA Motor Neurons, is Good Platform For Testing Possible Therapies, Study Suggests
A 3-D cell model derived from patients’ stem cells is able to mimic motor neurons from spinal muscular atrophy (SMA) patients and can become a better physiological tool to study disease mechanisms and screen therapy candidates, new research shows.
The study, “Cell cycle inhibitors protect motor neurons in an organoid model of Spinal Muscular Atrophy,” was published in Cell Death & Disease.
In most cases, SMA is caused by genetic mutations in the SMN1 gene, which lead to a steep drop in levels of survival of motor neuron (SMN) protein.
Although this protein is produced by many body tissues, it remains to be fully understood why motor neurons are one of the most severely affected cell types.
Based on animal studies and the fact that SMA onset can occur in the first months of life, it has been proposed that SMA is also a neurodevelopmental disorder “where motor neurons in the spinal cord do not properly form, and those that eventually survive would rapidly degenerate postnatally,” researchers said. But this hypothesis remains controversial.
Led by researchers at the National University of Singapore, the team addressed these questions by creating a laboratory cell model that allowed them to study the development and neurodegeneration of motor neurons from people with SMA.
Ask questions and share your knowledge of SMA in our forums.
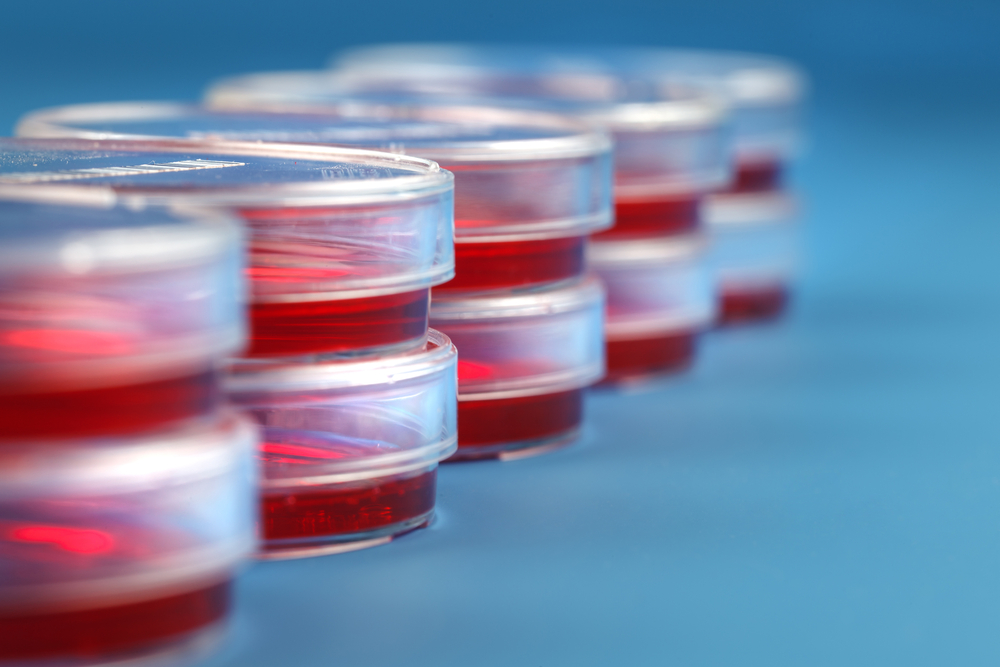
The model, called spinal neural organoids, is an “in vivo-like” three-dimensional model of motor neurons in the spinal cord derived from human induced pluripotent stem cells (iPSCs). These cells are derived from either skin or blood cells that have been reprogrammed back into a stem cell-like state, allowing for the development of an unlimited source of any type of human cell necessary.
Neural organoids are 3-D culture systems that give new form to the developmental processes and organization of the central nervous system, and have “immense potential for studying human neural development,” researchers said.
The scientists were able to derive spinal organoids from the cells of healthy people and SMA donors’ cells. These organoids contained many of the cells naturally present in the ventral spinal cord — motor neurons, astrocytes and interneurons — which was evidence that the model was suitable to mimic the natural in vivo environment of spinal nerves.
Using these organoids, scientists compared the development of motor neurons from healthy subjects with those from SMA patients. They found no alterations in the formation of both neural precursor cells or mature neurons, “highlighting that motor neuron formation is not impaired” in SMA, researchers said.
SMA motor neurons rapidly died after reaching maturity, and, importantly, the higher the SMA severity of patient donors (type 1 and type 2), the higher the severity of motor neuron loss in the spinal organoids.
Researchers also more closely examined the process of motor neuron cell death and found that motor neurons derived from SMA patients aberrantly reactivated cell replication. If replication was blocked by treating spinal organoids with a small molecule inhibitor, called a pan-CDK inhibitor, SMA motor neurons lived significantly longer.
“This confirmed that neural organoids are amenable for small molecule screening approaches and could be considered as an additional screening step before moving into in vivo models,” researchers said.
These 3-D models could also effectively reproduce the spectrum of SMA manifestations and be used to study how neurodegeneration happens.