Gene Therapy Delivered By Virus Shows Promise For Treating Spinal Muscular Atrophy (SMA)
Spinal Muscular Atrophy (SMA) is a genetic disorder that causes progressive muscle wasting and robs the afflicted of physical strength and leads to mobility impairment due to its effect on motor nerve cells in the spinal cord. SMA eventually results in loss of the ability to walk, eat, or breathe, and is the number one genetic cause of infant death worldwide, and the second most common inherited autosomal recessive disorder.
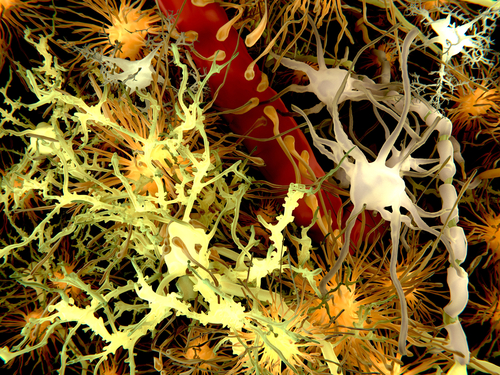
The disease is caused by a mutated or malfunctioning survival motor neuron 1 gene (SMN1) on the 5th chromosome. In healthy people, SMN1 produces the SMN protein, which is widely expressed in motor nerve cells, the eukaryotic cells critical to nerve function and muscle control. In SMN’s absence, motor nerve cells lose their capacity to function properly and eventually die, resulting in progressive and often fatal debilitation, muscle weakness, and difficulty performing basic life functions such as breathing and swallowing. Symptoms often manifest as weakness in controlling head and neck movements, with muscular control of limb movement also affected. Intellectual and cognitive abilities remain unaffected, in fact, older SMA patients tend to have higher IQs than average.
In SMA, disease severity is modified by the copy number of the SMN2 gene, a modified variant of the SMN1 that retains some functionality. A mutated SMN1 gene and no copy of the SMN2 gene will result in embryonic lethality.
SMA is a rare/orphan disease affecting approximately 1 in every 6,000-10,000 children born. The SMN gene is carried on chromosome 5, and in order for SMA to be inherited, both parents must carry a mutation in the SMN1 gene. If both parents carry gene mutations, there is a 25 percent chance that any of their children will manifest SMA. Roughly one-in-40 to one-in-80 normal men and women will be a genetic carrier, across all races and ethnicities.
The four main types of SMA — designated I, II, III, and IV — are distinguished by age of onset and peak physical milestone achieved. Typically, proximal muscles and muscles of the lung are first affected, and eventually other body systems as well, especially in early-onset types.
Type I SMA, also known as Werdnig-Hoffman disease, is the early-onset form, in which symptoms occur prior to 6 months of age. The most severe form of SMA, Type I accounts for 58 percent of SMA incidence at birth, and results in inability to sit without support, difficulty with breathing and swallowing, and is lethal for 90 percent of victims by two years of age.
[adrotate group=”3″]
Type II SMA, alternately known as Dubowitz disease, is characterized by onset at between six and 18 months of age, and is the second most prevalent form, accounting for 29 percent of SMA incidence at birth. Type II patients frequently have three copies of the SMN2 gene, and will vary in rapidity of disease progression. Typically, Type II patients will be able to sit but not to stand upright. Body muscles weaken, with respiratory system dysfunction a major concern. Life expectancy of Type II patients is somewhat reduced, but many survive into adulthood with careful medical attention.
Type III SMA, also known as Kugelberg-Welander disease or juvenile SMA, is juvenile-onset, with symptoms first manifesting when the patient is older than 18 months. Life expectancy with Type III is near normal, but persons affected may lose their ability to walk unassisted and have increased risk of developing scoliosis.
Type IV SMA, adult-onset SMA, is extremely rare, and begins to affect patients’ abilities at between 30 and 40 years of age. Life expectancy with Type IV SMA is normal, but patients may eventually need a wheelchair for mobility.
Currently there are no approved therapies for SMA, and current drug therapy has proved unsuccessful in stabilizing or reversing the disease. Consequently, treatment for SMA patients is supportive and palliative. Respiratory care is critical for Type 1 and Type 2 SMA patients, and assistive technologies for mobility and scoliosis are available.
Experimental Virus-Delivered SMA Therapy
However, Dallas-based clinic-stage gene therapy platform company AveXis is working to change that. Reformed in 2013, AveXis is very unique in that it was conceived to create academic and industry alliances for development of treatments for unmet medical needs, and SMA is the company’s first focus. AveXis and other biotech companies are pursuing research and development of SMA treatments including gene therapy, stem cell therapy, SMN2 upregulation, SMN2 splicing and SMN stabilization. Several clinical trials of therapies designed to affect SMA progression are also in progress, mainly for Type 1 and Types 2/3 of the disease.
AveXis got its start in Dallas, Texas and is financed by its founders along with PBM Capital from Charlottesville VA, Roche Venture Fund from Basel Switzerland, and Deerfield Management from NY, among others.
The company’s name, AveXis, which has both scientific and mythological meaning, is derived from scientific terms involved in the company’s work plus the name of a mythological figure. Hence, Av = adeno-associated virus (AAV) serotype 9; ve = vector; X = DNA helix; is = Isis, the goddess of children, nature and magic, who is particularly symbolic since the company’s initial focus, SMA, affects children, and because they hope to rework nature with a little magic (in the form of brilliant scientific discovery) to treat it.
This month, AveXis launched a new website specifically focused on SMA: https://www.smastudy.org — an integral element to AveXis’ multi-pronged effort to increase awareness of ongoing and upcoming SMA treatment clinical trials. While the company’s corporate website is centered on AveXis, the new SMA-focused website’s role will be to communicate directly with parents of children with SMA who are looking for worldwide information and guidance as well as treatment options available and not just information on AveXis and gene therapy.
The new website presents information about ongoing open enrollment in the Gene Transfer Clinical Trial for SMA Type 1 (NCT02122952), and about a gene therapy product developed by Dr. Brian Kaspar, of Nationwide Children’s Hospital, which has been licensed to AveXis for development and commercialization. The AveXis gene therapy biologic is currently referred to by its development internal code name “chariSMA.” There are also links to connect patients, parents, and families with resources like the several SMA focused organizations, foundations, and support and advocacy groups worldwide, as well as links to other clinical trials available for patients with all SMA types.
“It is very important for AveXis to remain rooted and communicate effectively to the community which is so supportive of our work in gene therapy. The intention of this new website is to empower people around the world to learn about SMA, to inform them of their clinical trial options, and to provide links to educational support organizations, which are always useful when looking for answers,” commented Mr. John A. Carbona, the Company’s Chief Executive Officer, on the website’s launch.
Early contributions to gene therapy at Nationwide Children’s was provided by Sophia’s Cure Foundation which is a non-profit public charity established by the Gaynor family in New York shortly after their daughter, Sophia, was diagnosed with Spinal Muscular Atrophy in 2009. The foundation was created to assist in funding for clinical research towards finding a cure for SMA and to offer support to families affected by this disease.
AveXis is also working with leading European medical research centers in the UK and France on teasing out the financial and regulatory hurdles that need clearance in order to initiate a mirror image of the chariSMA trial in Europe in 2015/2016. The company is also reaching out to domestic and international foundations and patient advocacy groups to increase overall awareness of their clinical trials
In addition, AveXis is launching its C.A.N. Program — a new initiative designed to “Contact All Neurologists” in order to increase awareness of ongoing and upcoming SMA clinical trials, and to inform neurologists as to how they can help shape future patient recruitment in SMA trials.
About AveXis’ Current SMA Type 1 Clinical Trial
The chariSMA (scAAV9.CB.SMN) approach is to introduce fully functioning copies of an SMN gene, intended to supplement the body’s SMN protein production. A particularly fascinating aspect of AveXis’ chariSMA gene transfer therapy is that it hitches a ride, so to speak, on the tiny virus — essentially harnessing a virus to deliver medicine. ChariSMA utilizes a non-disease causing virus (AAV9) to deliver the functional SMN gene to patients. In preclinical studies, AAV9 has been shown to cross the blood-brain-barrier, delivering SMN to motor neurons and significantly improve survival and motor function in an animal model of SMA.
According to AveXis, the newly introduced SMN gene exists in an episomal or extrachromosomal form, meaning that it will not integrate into the cell’s genome. The cell will begin continuous production of the SMN protein from new copies of the SMN gene.
A Phase 1 gene transfer clinical trial of AveXis’s chariSM A in SMA Type 1 infants is underway at Nationwide Children’s Hospital in Columbus, Ohio, which received IND approval and Fast Track designation from the FDA in September 2013, and Orphan Drug Designation this past October. “Fast track,” refers to a hastened phase in the drug review and approval process, and signifies that the FDA can expedite the review and development of chariSMA. Orphan Drug Designation is granted by the FDA Office of Orphan Drug Products to drugs intended to treat rare diseases or conditions affecting fewer than 200,000 people in the U.S. There are estimated to be between 25,000 and 50,000 SMA patients in the U.S., Europe and Japan.
The purpose of this Phase 1/2 (ClinicalTrials.gov Identifier: NCT02122952), single-site, dose-escalation study, is to evaluate the safety and efficacy of gene transfer in SMA Type 1. Participating patients are given a single viral intravenous infusion followed by careful monitoring for any side effects at outpatient follow-up visits at weekly intervals for three weeks, followed by monthly visits for the remainder of the two year active study period. Safety endpoints will be assessed by measuring changes in hematology, serum chemistry, urinalysis, immunologic response to rAAV9 and SMN, as well as reported history and symptoms observation. The time from birth to study pre-defined use of respiratory assistance devices or death will be used as a secondary outcome efficacy measure. Additional exploratory outcome measures will include nerve conduction and muscle assessment studies. The active phase of this study will extend two years post-infusion, after which participants will be asked to transfer into a monitoring program in which medical progress will continue to be collected from annual standard care medical exams for the next 15 years.
The Principal Investigator is Jerry R Mendell, MD, Director of the Center for Gene Therapy at The Research Institute at Nationwide Children’s Hospital. Dr. Mendell has over 35 years of clinical trial expertise. The first patient was enrolled and successfully injected with about 400 trillion viral particles containing the SMN transgene at Nationwide Children’s Hospital on May 13, 2014, and the trial’s estimated study completion date is June, 2017.
AveXis has announced modification of the current trial design with the addition of a third cohort that will receive a mid-range dose — marking a departure from the originally-designed 2-cohort trial.
“We are also on track to start our intrathecal trial in the first half of 2015 and very serious thought is being given to how we can treat Type 2 patients late 2015 or 2016,” noted AveXis’ Chief Scientific Officer Allan Kaspar, Ph.D.
This trial is currently recruiting participants, with an enrollment to be nine subjects. Subjects must be nine months of age or younger at the day of vector infusion with Type 1 SMA as defined by the following features:
1) Bi-allelic SMN1 gene mutations (deletion or point mutation) with two copies of SMN2 (no more and no fewer).
2) Onset of disease between birth and 6 months of age.
3) Hypotonia by clinical evaluation, with delay in motor skills, poor head control, round shoulder posture and hypermobility of joints.
Exclusion Criteria include:
1) Active viral infection (includes HIV or serology positive for hepatitis B or C)
2) Use of invasive ventilatory support (tracheotomy with positive pressure), or pulse oximetry <95% saturation. Patients may be put on non-invasive ventilator support (BiPAP) for less than 16 hours a day at the discretion of their physician or research staff.
3) Concomitant illness that in the opinion of the PI creates unnecessary risks for gene transfer
4) Concomitant use of any of the following drugs: drugs for treatment of myopathy or neuropathy, agents used to treat diabetes mellitus, or ongoing immunosuppressive therapy or immunosuppressive therapy within 3 months of starting the trial (e.g. corticosteroids, cyclosporine, tacrolimus, methotrexate, cyclophosphamide, intravenous immunoglobulin, rituximab)
5) Patients with Anti-AAV9 antibody titers >1:50 as determined by ELISA binding immunoassay.
6) Abnormal laboratory values considered clinically significant (GGT > 3XULN, bilirubin 3.0 mg/dL , creatinine 1.8 mg/dL, Hgb < 8 or > 18 g/Dl; WBC > 20,000 per cmm)
7) Participation in a recent SMA treatment clinical trial that in the opinion of the PI creates unnecessary risks for gene transfer.
8) Family does not want to disclose patient’s study participation with primary care physician and other medical providers.
9) Patient with signs of aspiration based on a swallowing test and unwilling to use an alternative method to oral feeding.
[adrotate group=”3″]
Early contributions to gene therapy at Nationwide Children’s was provided by Sophia’s Cure Foundation which is a non-profit public charity established by the Gaynor family in New York shortly after their daughter, Sophia, was diagnosed with Spinal Muscular Atrophy in 2009. The foundation was created to assist in funding for clinical research towards finding a cure for SMA and to offer support to families affected by this disease.
AveXis is also working with leading European medical research centers in the UK and France on teasing out the financial and regulatory hurdles that need clearance in order to initiate a mirror image chariSMA trial in Europe in 2015. The company is also reaching out to domestic and international foundations and patient advocacy groups to increase overall awareness of their clinical trials
In addition, AveXis is launching its C.A.N. Program — a new initiative designed to “Contact All Neurologists” in order to increase awareness of ongoing and upcoming SMA clinical trials, and to inform neurologists as to how they can help shape future patient recruitment in SMA trials.
For more information about AveXis:
https://avexisinc.com
Sources:
AveXis Inc.
Nationwide Children’s Hospital
ClinicalTrials.gov
Sophia’s Cure Foundation
CureSMA.org
Wikipedia
Image Credits:
AveXis Inc.
Nationwide Children’s Hospital