Abnormal immune system activation seen in SMA fly models
Researchers say mechanism may contribute to neurodegeneration in disease
Written by |

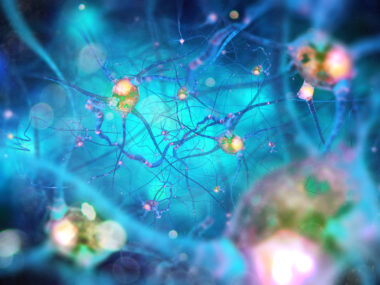
A range of genetic mutations associated with spinal muscular atrophy (SMA) were linked to abnormal activation of the immune system in fly models, which a team of U.S. researchers believe could be a mechanism that contributes to neurodegeneration in the rare disease.
Altogether, the evidence indicated that these exacerbated immune responses were a consequence of the loss of SMN, the protein that SMA patients lack. Moreover, the more severe a disease-causing mutation, the greater the immune activation, according to the researchers.
“In alignment with recent research on other neurodegenerative diseases, these findings suggest that hyperactivation of innate immunity contributes to SMA,” the team wrote.
The study, “Dysregulation of innate immune signaling in animal models of spinal muscular atrophy,” was published in BMC Biology.
Investigating the mechanisms of immune system activation in SMA
The most common types of SMA are caused by mutations in the SMN gene, leading to a lack of the SMN protein. Patients experience progressive muscle weakness and wasting due to the degeneration of the specialized nerve cells in the spinal cord involved in voluntary movement.
SMA severity varies by disease type, with less SMN protein linked to more severe disease and an earlier age of onset among patients.
SMN is involved in the processing of RNA — a type of genetic template molecule used to make proteins. The cellular mechanisms that explain exactly how its loss triggers neurodegeneration in SMA are still being explored.
Recent research has pointed to a role for the immune system. Studies have shown abnormal development of immune cells and organs in mouse models of SMA that precede nerve cell loss, and dysregulation of the immune system has also been observed in pediatric SMA patients, according to the authors.
In Drosophila or fruit fly models housing various SMA-associated mutations, a team of researchers from the University of North Carolina at Chapel Hill previously found a gene activity signature suggesting an overactivation of the innate immune system, the branch of the immune system that serves broadly as a first responder to potential threats. These responses were most pronounced in flies with mutations linked to more severe disease.
Now, the scientists returned to the fly models to further explore these relationships. They looked at both gene activity and protein levels in flies with SMA-associated mutations with ranging severity.
Again, the team recognized a signature of innate immune activation in the SMA models relative to healthy flies, even in those with less severe mutations, although evidence of greater immune activation was seen in flies with more severe disease. This immune system activation was happening even without a distinct external force, such as exposure to a pathogen, to drive it.
In particular, the flies experienced increases in proteins associated with defense responses against bacteria, fungi, and viruses, as well as melanization. Melanin is the pigment that gives hair, eyes, and skin a darker color. These fruit flies produce it as an immune defense response to encapsulate harmful invaders.
According to the researchers, the SMA flies commonly exhibited pigmented nodules, or melanotic masses, or cell clumps associated with the defense process.
“These structures typically form in response to pathogens, tissue damage, and necrosis [tissue death], but this defense response can also be triggered by different genetic perturbations,” the researchers wrote.
Greater immune activation seen with more severe disease
As seen with the molecular immune signatures, more melanotic masses were evident in flies with a more severe disease presentation.
Further experiments indicated that the observed immune dysregulation appeared to be a primary consequence of SMN loss in immune cells and tissues.
A series of other experiments showed a few specific immune proteins and pathways that appeared to be disrupted by SMN loss and might contribute to immune activation.
Overall, the researchers believe the findings suggest that aberrant immune activation in SMA might contribute to neurodegeneration in the disease, as has been seen in a range of other neurodegenerative conditions.
Although the precise mechanisms remain unclear, neuroinflammatory responses like those identified here are likely to contribute to the pathophysiology [mechanisms] of neurodegenerative diseases like spinal muscular atrophy.
Still, the scientists noted that more work is needed to identify how significant of a role the immune system plays in SMA, and which particular immune proteins are most implicated.
“Although the precise mechanisms remain unclear, neuroinflammatory responses like those identified here are likely to contribute to the pathophysiology [mechanisms] of neurodegenerative diseases like spinal muscular atrophy,” the team concluded.