SMA Research Review Shows How Disease Phenotype, Mouse Models are Leading to Therapeutic Strategies
Written by |

 A recent review entitled “Neurodegeneration in spinal muscular atrophy: from disease phenotype and animal models to therapeutic strategies and beyond,” recently published the journal Future Neurology, discussed current evidence on SMA with a specific focus on the existing treatment options.
A recent review entitled “Neurodegeneration in spinal muscular atrophy: from disease phenotype and animal models to therapeutic strategies and beyond,” recently published the journal Future Neurology, discussed current evidence on SMA with a specific focus on the existing treatment options.
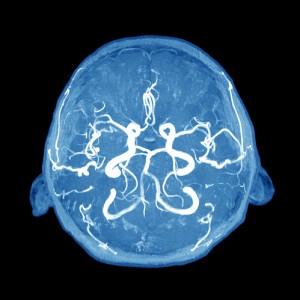
Spinal muscular atrophy (SMA) is an autosomal recessive neuromuscular disorder that affects the pediatric population, with an estimation of nearly 10,000 afflicted newborns. SMA patients exhibit a characteristic muscle weakness that affects the proximal muscles more than it does the distal ones, the lower limbs more than the upper ones, and intercostal and axial muscle groups more than the diaphragm. Recent data from studies of SMA mouse models suggest that defects of the neuromuscular synapses are perhaps the earliest pathological hallmarks of the disease.
The causes of SMA remain poorly understood, however, recent findings indicate that a strong basis of molecular genetic alterations in the SMA pathogenesis, especially the involvement of the SMN1 gene that was found to be mutated in SMA.
[adrotate group=”3″]
Sequence analysis determined that the SMN1 gene lay within an inverted duplication that also contains an almost identical homolog, SMN2. As mentioned, SMA patients have mutations and/or deletions in the SMN1, but also carry one or more copies of the SMN2 gene. The difference between the two SMN genes is a nucleotide change inside exon 7 that alters the efficiency with which exon 7 is included within the SMN transcript, creating an exonic splicing suppressor in the SMN2 gene. These conclusions led to an encouraging increase in studies aimed at developing potential treatments for SMA based on the SMN2 molecular target.
In this regard, in their review, Umrao R Monani and Darryl C De Vivo from the Columbia University Medical Center, New York, USA describe existing treatment options for an effective treatment for the disease.
Restoring SMN by manipulating SMN2 has driven the study for treatments for options. Studies with US FDA-approved small molecules, such as histone deacetylase inhibitors, have been tested in mice models of SMA with some degree of therapeutic benefit. These reagents are currently either being modified for safety or being tested in clinical trials. The most promising treatment involves the use of antisense oligonucleotides, potent splice modulators that are also presently being tested. If the results in mice are any measure of the effects of these molecules in patients, the outcome may be promising.
The researchers concluded that additional research to elucidate the molecular mechanisms underlying human SMA must be refined to improve current available therapies.