FAQs about symptoms of SMA
Adults and children are affected differently by spinal muscular atrophy (SMA). SMA types with an onset in childhood (types 0–2) tend to have more severe symptoms than types in which symptoms appear later on (types 3–4).
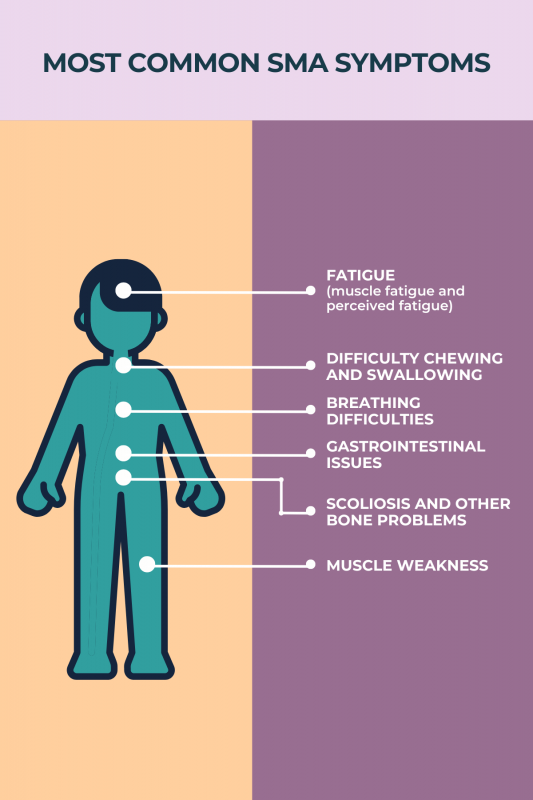
Because spinal muscular atrophy (SMA) is marked by the progressive loss of nerve cells needed for voluntary movement, symptoms such as muscle weakness, breathing problems, and scoliosis (an abnormal and progressive sideways curvature of the spine), tend to worsen over time. How much and how quickly spinal muscular atrophy symptoms progress will depend on a person’s SMA type, with milder types usually progressing more slowly than more severe types.
Some lifestyle changes, in combination with spinal muscular atrophy (SMA) treatment, may help ease SMA symptoms. A regular exercise regimen and/or physical therapy, established with a patient’s healthcare team, can help to improve mobility and ease fatigue. While there is no established SMA diet, maintaining sufficient nutrition with the help of one’s healthcare providers can support muscle strength and healthy growth.
Symptom onset in spinal muscular atrophy (SMA) depends on the disease type, with more severe forms of SMA generally associated with an earlier start of symptoms. Of the five main SMA types, the most severe (type 0) is marked by symptoms that appear in utero, or before birth, whereas symptoms in the most mild form (type 4) typically emerge in adulthood.
For patients with more severe types of spinal muscular atrophy (SMA) with symptom onset before birth or in childhood, a failure to meet certain motor milestones or a lack of fetal movements will usually prompt doctors to suspect SMA. For patients with mild, adult-onset types of SMA, it may take more time to reach a diagnosis. People experiencing any unexpected symptoms or changes in their health status should seek the advice of a healthcare professional.
 Medically reviewed by
Medically reviewed by