FAQs about SMA diagnosis
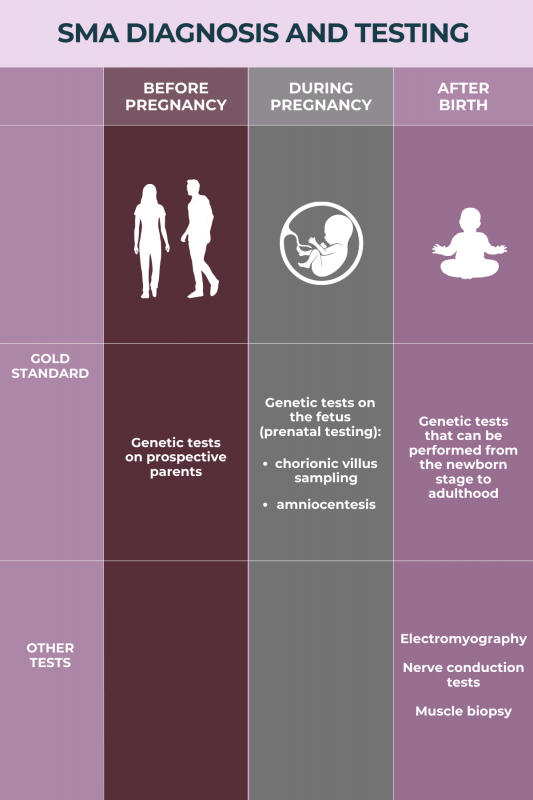
The gold standard for diagnosing spinal muscular atrophy (SMA) is genetic testing to identify disease-causing mutations. The main forms of SMA are caused by mutations in the SMN1 gene, but mutations in other specific genes can result in less common forms of the disease. Other tests may be performed as part of a diagnostic workup.
Spinal muscular atrophy (SMA) can be diagnosed at any age. Because the mutations that cause SMA are present from the moment of conception, or when a sperm cell fertilizes an egg cell, testing and diagnosis of the disease may be performed even while a developing fetus is still in the womb. However, many patients are only diagnosed at the time of symptom onset, which differs between SMA types, or as part of newborn screening programs for the main types of SMA (types 0 to 4).
Genetic testing for spinal muscular atrophy (SMA) is a medical laboratory technique that checks whether a person carries mutations that are known to cause SMA. Genetic testing also can be used to identify SMA carriers — people who will not develop SMA themselves, but who carry the disease-causing mutation and may pass it on to their biological children.
Genetic disorders such as spinal muscular atrophy (SMA) can be detected during pregnancy by taking a small sample of cells from the fetus and performing genetic testing to look for disease-causing mutations. The most common strategies used to obtain fetal cells for this testing are chorionic villus sampling (CVS), which collects a sample of cells from the placenta, and amniocentesis, which takes a sample of the fluid surrounding the developing fetus.
Without an accurate diagnosis, it is impossible to administer the appropriate treatment. Consequently, patients who have spinal muscular atrophy (SMA) but are not diagnosed will continue to experience disease progression, with symptoms such as muscle weakness and breathing problems continually getting worse over time. Once SMA is diagnosed, therapies are available for the main types of SMA (types 0 to 4) that can be administered to help slow or stall the progression of the disease.
Related Articles

 Medically reviewed by
Medically reviewed by