Potential Therapeutic Target Against SMA is Identified
Neurochondrin, a protein essential for nerve cells, was found to interact with the survivor motor neuron protein (SMN), whose deficiency causes spinal muscular atrophy (SMA). This finding reveals a previously unknown player and potential therapeutic target for SMA.
The study “Neurochondrin interacts with the SMN protein suggesting a novel mechanism for Spinal Muscular Atrophy pathology” was published in the Journal of Cell Science.
Although SMA can be caused by mutations in different genes, most patients have inherited mutations in the SMN1 gene, which instructs the body to produce the protein SMN. As a result, SMN1 mutations lead to a shortage of the SMN protein, resulting in death of motor neurons, and impairing transmission of nerve impulses between the brain and the muscles.
One of the reasons behind the lack of treatment options for SMA is uncertainty about the roles of SMN, which appear to be diverse. In particular, it is unclear why a deficiency in SMN protein affects primarily motor neurons, given that its functions appear to be necessary for all cell types.
SMN is important for the correct production and transport of messenger RNAs, which are intermediary molecules that convey genetic information from DNA to proteins.
Its role in cellular transport is thought to be linked with the conversion of messenger RNA into proteins at certain distant places in the cell. This seems to be particularly important for motor neurons, which bear long axons (neuron projections that conduct impulses and allow communication with other nerve cells).
SMN partners with other proteins, called Sm proteins, to perform its functions.
Researchers used neuron-like cells cultured in the laboratory and searched for other molecules that interacted with SMN. They identified one called neurochondrin, about which little is known besides that it is essential for neuron growth and communication.
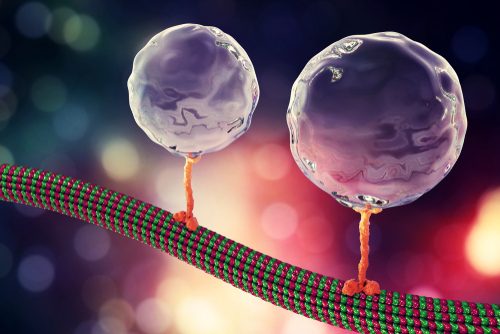
Researchers found that neurochondrin interacts with SMN and Sm proteins in vesicles that move inside nerve cells. Importantly, neurochondrin is strongly expressed in motor neurons in the spinal cords of mice, suggesting it plays a particularly important role in these cells.
When SMN protein levels were artificially lowered in cells, mirroring what happens in people with SMA, neurochondrin could not acquire its normal localization in vesicles.
This suggests that the low levels of SMN present in SMA patients, also can compromise the function of neurochondrin and impact disease development.
The research team thinks that SMN-neurochondrin vesicles can be involved in exchanging messenger RNAs and proteins along the cell, which is particularly relevant in elongated cells such as motor neurons.
“Neurochondrin warrants further investigation in the context of SMA pathology and may prove useful as a target for future therapy development,” researchers wrote.
Further work is required to establish if neurochondrin is relevant for SMA and can be explored for therapeutic purposes. However, the team believes that neurochondrin may have potential as a therapeutic target for SMA together with, or in place of it, for patients for whom it is not suitable, treatments targeting SMN expression such as Biogen’s Spinraza (nusinersen).







