Blood Test for SMN Protein Levels May Help Monitor Treatment Response in SMA, Study Reports
Researchers in Japan have developed a non-invasive test to measure levels of the SMN protein using cells circulating in the blood of spinal muscular atrophy (SMA) patients. The test is a potentially useful tool in monitoring treatment response.
The results of the study, “A new biomarker candidate for spinal muscular atrophy: Identification of a peripheral blood cell population capable of monitoring the level of survival motor neurone protein” were recently published in the open-access journal PLOS one.
SMA is caused by mutations in the survival motor neuron 1 (SMN1) gene that result in an absent or non-functioning SMN protein. Loss of this protein leads to the selective loss of motor neurons in the spinal cord, which causes muscles to weaken and die (atrophy).
Therapeutic options include ways to increase SMN protein levels by addressing problems in the SMN1 gene — the primary source of the SMN protein — or by targeting SMN2, which also encodes for this protein.
A first disease-modifying SMA therapy, Spinraza (nusinersen), developed and marketed by Biogen, was approved to treat all disease types in 2016. Others, including the gene therapy AVXS-101 and risdiplam, which, like Spinraza, targets the SMN2 gene, are in clinical testing.
Ask questions and share your knowledge of SMA in our forums.
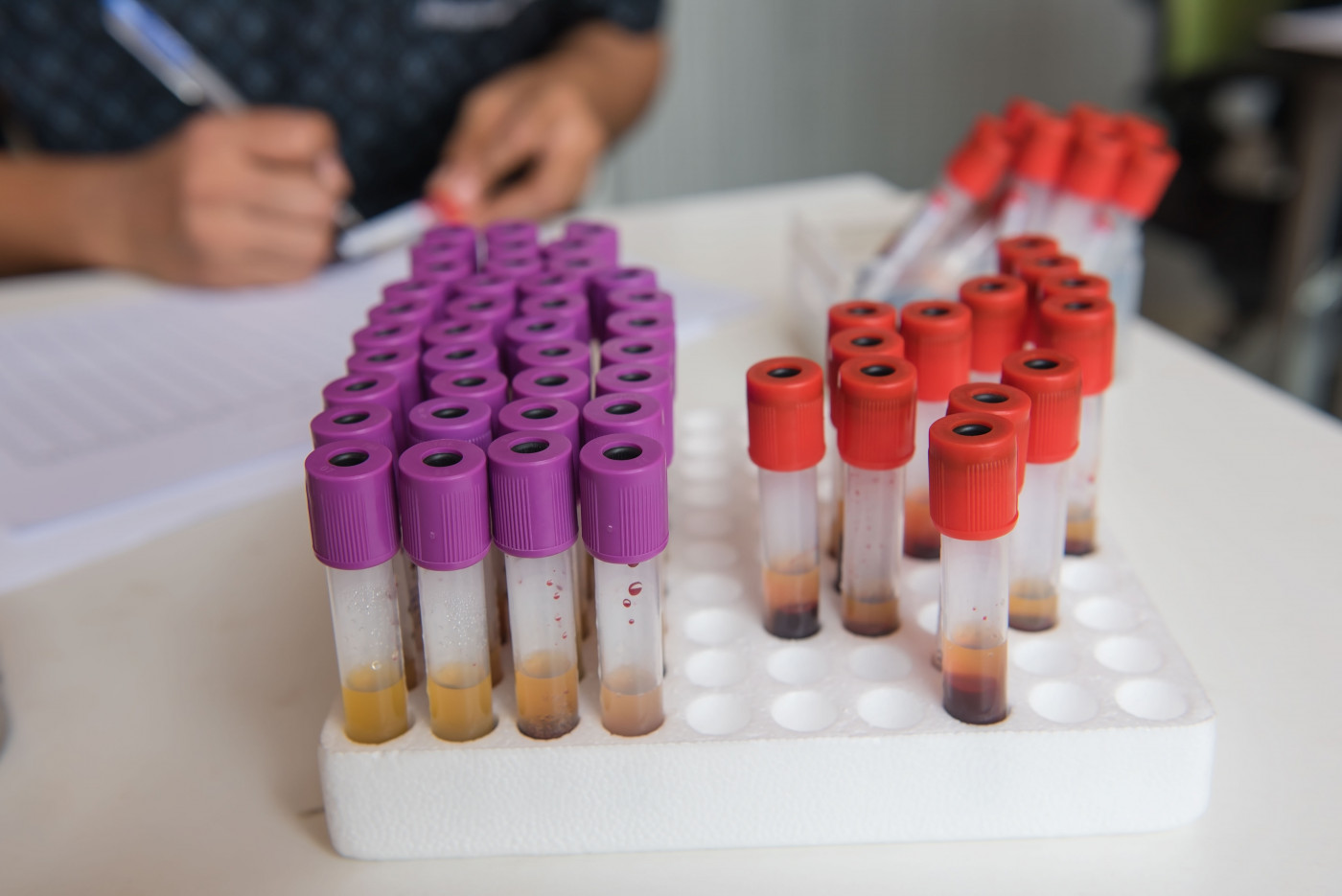
To evaluate how well a therapy is working, clinicians need ways to measure levels of the SMN protein. Looking at levels in a patient’s spinal cord, where SMN is needed most, is not a realistic option, but levels in the peripheral blood — circulating blood — might be a good alternative. There are currently several different methods to evaluate SMN levels in different cells or tissues.
Researchers in Tokyo used a new approach that looked at SMN protein levels in cells found in the peripheral blood and treated with a fluorescent dye. They used a technique called imaging flow cytometry. Flow cytometry is known for its ability to measure characteristics of individual cells as they are passed through a laser. Imaging flow cytometry combines conventional flow cytometry with a powerful microscope able to visualize individual cells.
Twenty-five SMA patients, with types 1 to 3 and ranging in age from 2 months to 60 years, were enrolled and their peripheral blood analyzed for SMN expression (in four different cell types). Important in terms of validating this approach, SMN protein levels were seen to be lower in three of these cell populations (T cells, B cells, and monocytes) in SMA patients compared to healthy controls.
Previous studies have shown that the SMN protein concentrates at specific “spots” in the nucleus of each cell. Using imaging flow cytometry, researchers could identify and quantify these spots. The spots were particularly prevalent in monocyte cells, the study reported, and again the number of these spots was significantly lower in patients than controls.
“There were no significant differences in the data between adults and infants, for either control or SMA subjects,” the researchers said. “These results indicate that the levels of SMN protein expression in PBCs [peripheral blood cells] can be compared using imaging flow cytometry.”
The number of these spots and their intensity in SMA patients also correlated with disease severity, with “a significant difference between type I and type III … in the percentages of SMN-spot+ cells” observed. For example, two patients with very limited motor skills had a relatively low number of SMN spots, the study reported.
More research needs to be done to validate this approach. But “we anticipate that SMN spot analysis will become the primary endpoint for monitoring therapeutic intervention, serving as a biological marker of SMA therapeutic efficacy,” the research team concluded.