High adherence to Evrysdi linked to lower patient healthcare costs
Lowest adherence for ages 6-12, those with SMA type 4: Real-world study
Written by |
Nonadherence of spinal muscular atrophy (SMA) patients to their prescribed regimen of Evrysdi (risdiplam) — an oral solution generally taken once daily after a meal — is associated with higher healthcare costs, particularly in patients with type 2 disease.
That’s according to a real-world study in the U.S., which also reported that nonadherence to treatment, defined as taking the medication less than 80% of the days during the study, was higher among individuals with SMA type 4, also called adult-onset or late-onset SMA, and patients ages 6 to 12.
“These findings underscore the importance of treatment adherence and persistence for patients with SMA receiving [Evrysdi], particularly for younger children and those with greater disease severity,” the researchers wrote.
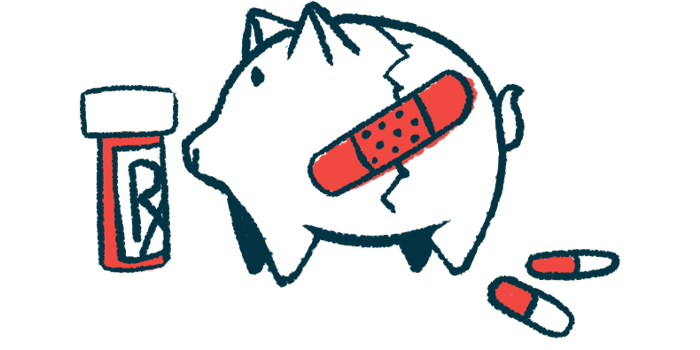
Overall, “our study found that patients who were highly adherent to [Evrysdi] … incurred $7,106 lower median [healthcare] costs than patients who were adherent to a lesser extent,” the team wrote, noting that these results “[highlight] the relationship between medical service costs and the extent of adherence to the treatment regimen.”
The study, “Risdiplam utilization, adherence, and associated health care costs for patients with spinal muscular atrophy: a United States retrospective claims database analysis,” was published in the Orphanet Journal of Rare Diseases. The work was funded by Novartis Gene Therapies, the maker of Zolgensma, a one-time gene therapy widely approved for SMA.
Investigating impact of Evrysdi adherence on healthcare costs in real world
SMA is caused primarily by mutations in the SMN1 gene that lead to a deficiency of the survival motor neuron protein, known as SMN. This results in progressive muscle weakness and wasting, and speaking, swallowing, and breathing problems.
Evrysdi is a disease-modifying therapy approved for people with SMA that works to increase the levels of functional SMN throughout the body. Marketed by Roche and its subsidiary Genentech, it is approved in the U.S. to treat all types of SMA in patients of all ages. Its efficacy depends on patient adherence to the treatment regimen and its continued use.
According to researchers, however, “there is limited real-world evidence of the adherence or persistence with [Evrysdi] for patients with SMA, or the impact of nonadherence on patients’ [healthcare] costs.”
To know more, researchers at Novartis Gene Therapies retrospectively analyzed data from a U.S. health insurance claims database from January 2020 through June 2022. That analysis involved 86 patients, more than half of them female. Among them, a majority — 47 individuals or 55% — had SMA type 3. The mean age of these patients was 17.3.
A total of 20 patients (about 23%) had a diagnosis of SMA type 4 and a mean age of 38.2. SMA type 2 affected 18 patients, who had a mean age of 7.9. The sole patient with SMA type 1 in the study was a 1-year-old boy.
Generalized muscle weakness was present in two-thirds of the participants with SMA type 2, and about one-quarter of those with SMA type 3 and type 4. Moreover, nearly three-quarters of patients with type 2 and 3 disease had scoliosis, or an abnormal curvature of the spine, and about 45% had shortness of breath and other respiratory difficulties.
Regarding treatment regimens, half of the patients were treated with Evrysdi only, while 42 had switched to Evrysdi after initial treatment with Spinraza (nusinersen), an injection therapy also approved for SMA. One patient received both Spinraza and the gene therapy Zolgensma (onasemnogene abeparvovec-xioi) before starting Evrysdi.
Treatment adherence, assessed as the proportion of days in which the medication was taken divided by the number of days in the study period, was 0.89 overall. However, it varied according to SMA type and a patient’s age. Adherence was highest in the boy with SMA type 1 (0.97), followed by patients as old as 2 years (0.96). It was lower (0.88) in those with SMA type 4, and lowest — 0.85 — among patients ages 6 to 12.
The analysis found that “the majority (83.7%) of patients were adherent,” meaning they had Evrysdi adherence of at least 0.8, though that percentage varied across SMA types.
Overall, the researchers found a higher proportion among younger patients (up to age 2; 100%) and a lower proportion in those ages 6 to 12 years (76.5%). Adherence also was lower in patients with SMA type 4, at 75%.
Within one year after starting treatment with Evrysdi, 18 patients (21%) discontinued the treatment. The proportion of patients that remained on treatment decreased rapidly after 60 days in participants with type 4 disease.
Healthcare costs for nonadherent SMA type 4 patients 16 times higher
Compared with adherent patients, those who did not stick to their treatment regimen had a higher total median healthcare cost due to all causes, the analysis found.
Overall, patients described as “highly adherent” by researchers were found to incur healthcare costs that were a median of about $7,000 less than those who were adherent to a lesser extent.
Relative to participants who adhered to therapy within each disease type, nonadherent individuals with type 4 SMA had three times higher costs: $16,817 vs. $4,594. Those with type 3 SMA who did not adhere to their regimen had fourfold greater healthcare costs, paying $56,113 versus $14,909 for those who were adherent.
The greatest difference was seen for patients with SMA type 2. Those who were nonadherent had median healthcare costs 16 times higher than those sticking to their prescribed regimen. The difference was $356,524 versus $21,475 in median costs.
An important finding of this study is that patients with SMA types 2, 3, or 4 who were nonadherent to their [Evrysdi] regimen incurred greater total [healthcare] costs compared with their adherent counterparts.
Similar results were seen regarding all-cause medical service costs. Also, the level of adherence to treatment impacted healthcare costs, as they were 1.6 times higher in patients with a treatment adherence between 0.80 and 0.90, compared with those with an adherence higher than 90%.
“An important finding of this study is that patients with SMA types 2, 3, or 4 who were nonadherent to their [Evrysdi] regimen incurred greater total [healthcare] costs compared with their adherent counterparts,” the researchers wrote.
The researchers noted that “medication nonadherence can negatively impact treatment effectiveness.” To that end, they wrote, “worsened clinical outcomes may result in … lower health-related quality of life, and more frequent health care resource use.”
The team called for “additional research with a larger sample size and longer follow-up … to further examine the long-term impact of real-world adherence to [Evrysdi] on patient outcomes.”
Such studies also should seek to “identify effective interventions for improving adherence,” the scientists wrote.