Spinraza treatment improves motor function in nonambulatory SMA
Gains seen over 4 years for children and adults in real-world analysis
Written by |
Treatment with Spinraza (nusinersen) improved motor function in children, adolescents, and adults with spinal muscle atrophy (SMA) who were unable to walk without assistance, according to a four-year real-world analysis.
Moreover, nine of the 12 patients who underwent continuous evaluations while on Spinraza over the four years achieved “clinically important differences” on one rating scale of motor function, the analysis found.
Such gains in motor function, as determined overall by a variety of standardized assessment tools, paralleled improvements in various activities of daily living, as indicated by interviews with patients and caregivers.
“As demonstrated by our findings, it is necessary to consider various functional aspects to determine the effectiveness of [Spinraza] therapy,” the researchers wrote.
The study, “Improvement in functional motor scores in patients with non-ambulatory spinal muscle atrophy during Nusinersen treatment in South Korea: a single center study,” was published in BMC Neurology.
Study used variety of tools to assess effects of Spinraza treatment
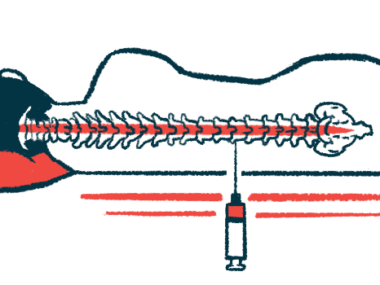
Spinraza is an injection therapy widely approved for children and adults with SMA. It works by increasing levels of the SMN protein, which is deficient in SMA patients, and helps to slow or halt the hallmark disease symptoms of progressive muscle wasting and weakness. The therapy is most effective when given before the signs of muscle weakness arise.
In this report, researchers in South Korea shared their experiences with Spinraza treatment over four years in a dozen nonambulatory SMA patients, 75% of whom were female. Nonambulatory means these patients were unable to walk or stand without assistance.
To gauge Spinraza’s effectiveness, patients underwent a series of standardized tests before treatment and about every four months thereafter. The main tests were the Hammersmith Infant Neurological Examination, or HINE, and the Hammersmith Functional Motor Scale Expanded, called HFMSE.
Based on pretreatment functional abilities, some patients were also assessed using other evaluations. Two standardized measures of motor function, both from the Children’s Hospital of Philadelphia, were used: CHOP INTEND (for Infant Test of Neuromuscular Disorders) and CHOP ATEND (or the Adult Test of Neuromuscular Disorders). Also employed were the Revised Upper Limb Module, known as RULM, and the Motor Function Measure, or MFM.
“This study stands out as the first to present results from serial evaluations using various assessment tools on the same patients, particularly those with non-ambulatory SMA,” the researchers wrote.
Seven patients received Spinraza during childhood or adolescence; five were treated as adults. Among them, 10 were diagnosed with SMA type 2, one with type 1, and another with type 3. Regarding functionality, 10 (83.3%) could sit, and two were non-sitters (16.7%). Three patients underwent surgery to correct scoliosis, a sideways curvature of the spine.
Based on HFMSE scores, nine patients (75%) reached a minimal clinically important difference (MCID), defined as an improvement of three points or more compared with pretreatment scores. The remaining three patients who did not achieve MCID were all adults. Despite no HFMSE gains, one of these adult patients showed improvements in CHOP-INTEND, CHOP-ATEND, and RULM.
This study stands out as the first to present results from serial evaluations using various assessment tools on the same patients, particularly those with non-ambulatory SMA. … [It] provided insights into the improvement and patterns of change of various functional assessment tools in non-ambulatory SMA after [Spinraza] treatment
Regarding changes over time, children and adolescents showed the most prominent improvement in CHOP-INTEND (mean 2.215-point increase/year), followed by HFMSE (mean 1.706-point increase/year). CHOP-INTEND scores in this group demonstrated a significantly higher rate of improvement compared with HINE, RULM, and MFM assessments.
CHOP-ATEND for adults also showed a statistically significant improvement over time (mean 0.912 points/year).
Based on interviews with patients and caregivers, gains in motor function scores were accompanied by improvements in various activities of daily living, known as ADLs. Such ADLs consisted of physical activity, dressing, mobility, self-care, self-feeding, reaching, picking up and holding objects, writing and technology use, social engagement, toileting, and work/school activities.
“This study provided insights into the improvement and patterns of change of various functional assessment tools in non-ambulatory SMA after [Spinraza] treatment,” the researchers concluded.
The team added that “focusing on the improvement of related ADLs is necessary to objectively assess the therapeutic effect and ensure meaningful improvement in the patients’ daily lives.”