Steps Taken by Stem Cells in Becoming Neurons Identified in Study, Aiding Cell Replacement Therapies
Written by |
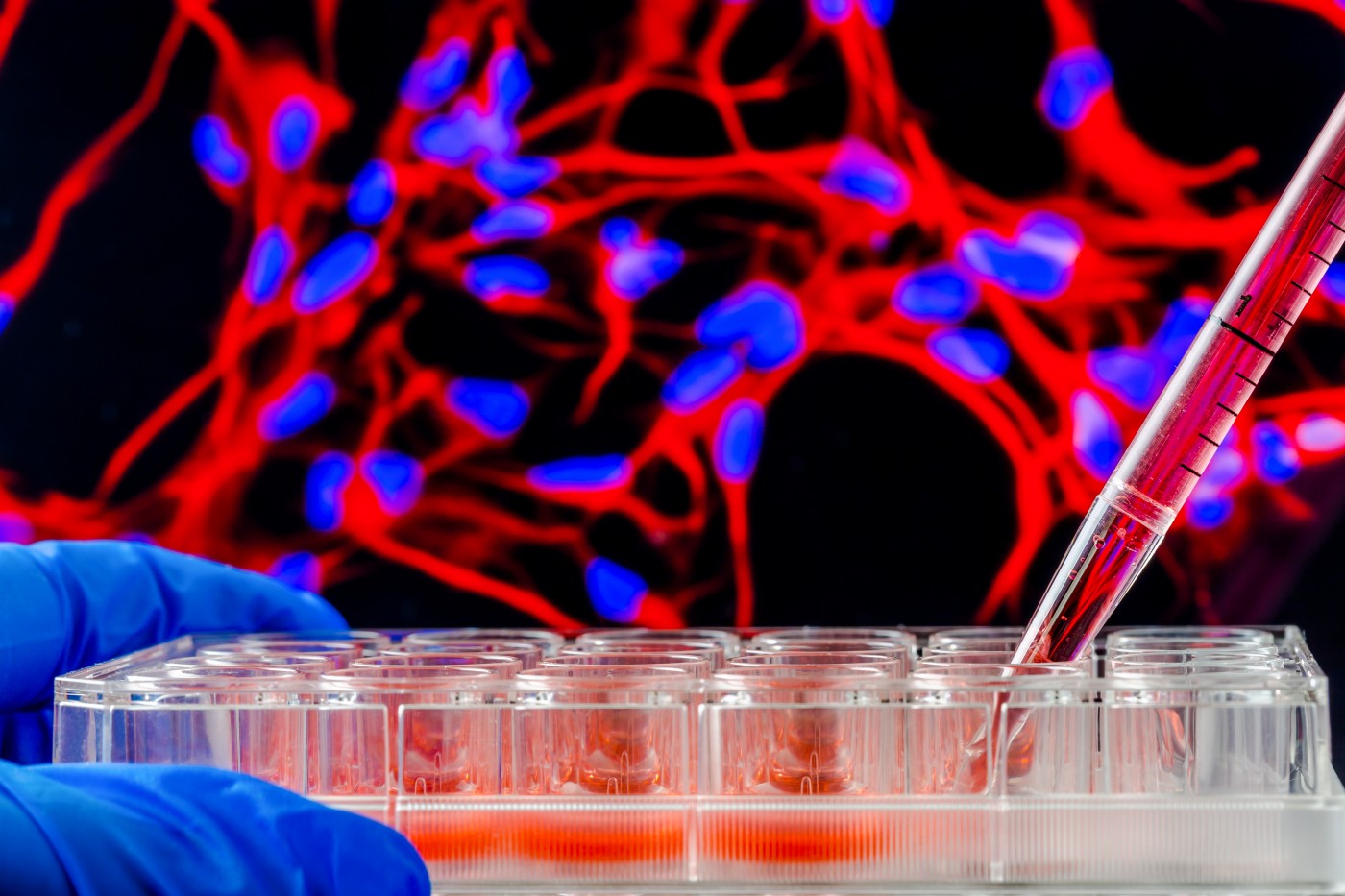
Researchers have become quite good at making stem cells grow into neurons in the lab, even without fully understanding the actual cellular processes that accompany the transition. Now, a study describes the sequence of events that make a signaling nerve cell out of an immature stem cell — knowledge that will be needed to, one day, use the technique to replace neurons lost to diseases such as spinal muscular atrophy (SMA).
The study, “A Multi-step Transcriptional and Chromatin State Cascade Underlies Motor Neuron Programming from Embryonic Stem Cells,” was published in the journal Cell Stem Cell.
Researchers also hoped that the insights from direct reprogramming of neurons may be used to generate other cell types.
“Despite having a great therapeutic potential, direct programming is generally inefficient and doesn’t fully take into account molecular complexity,” Esteban Mazzoni, an assistant professor in New York University‘s Department of Biology, and one of the study’s senior investigators, said in a news release.
“However, our findings point to possible new avenues for enhanced gene-therapy methods,” he added.
In earlier research, the team succeeded in improving the procedure’s efficiency. Identifying three transcription factors — molecules that control the activity of a large number of genes — the researchers used those factors to turn stem cells into neurons in two days, with a success rate of up to 95 percent.
But this direct programming is drastically different from what occurs in a developing embryo, in which stem cells go through several intermediate steps before becoming mature neurons, Uwe Ohler — another senior contributor from the Max Delbrück Center for Molecular Medicine (MDC) in Germany — explained.
So the team started observing the cells during the process. They learned that two of the factors worked together in the early stages of the transformation. By binding to the cells’ DNA, these factors activated a host of genes and triggered changes in the chromatin structure (the packaging of DNA into chromosomes).
Later on, the third factor comes in to activate additional genes, and, finally, the first two return to use the changes initiated by the third factor and complete the transformation.
Mazzoni explained that many researchers see direct programming as an attractive option, as it can potentially be used inside the body to replace damaged cells.
“However, questions remain about its viability to repair cells — especially given the complex nature of the biological process,” he said, specifying that direct programming lacks “the progression through intermediate stages” that the researchers had witnessed. Nevertheless, the team thinks this newfound knowledge can be used to “manipulate cells,” and develop cell replacement therapies for diseases such as SMA.



