European SMA Advocates Question EU’s Willingness to Reimburse for Zolgensma
Written by |

Hundreds of SMA patients and their caregivers gather in Warsaw in 2018. (Photo by Larry Luxner)
Now that the U.S. Food and Drug Administration has given its blessing to the AveXis gene therapy Zolgensma for children up to 2 years old with spinal muscular atrophy, the company hopes to win similar approval from the European Medicines Agency (EMA) later this year.
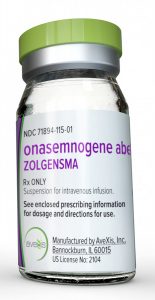
AveXis, which was acquired by Swiss pharma giant Novartis last year for $8.7 billion, submitted a marketing authorization application to the EMA in October 2018. Zolgensma (onasemnogene abeparvovec-xioi) is being evaluated under an accelerated assessment, which slashes the time frame for the review from 210 to 150 days.
“The medicine is currently under evaluation and we cannot speculate at this point about when the EMA will issue an opinion,” a spokeswoman for the agency told SMA News Today.
Farah Bulsara Speer, vice president of corporate communications at AveXis, confirmed the application but declined to say when the therapy might actually win approval from the Amsterdam-based EMA, which operates as a decentralized scientific agency for the 28-member European Union as well as Iceland, Liechtenstein, and Norway.
“We have been saying the second half of 2019,” she said. “We have not shared any further information beyond that time frame.”
Kacper Rucinski, a London-based executive board member of the nonprofit group SMA Europe, said the EMA is scrutinizing every aspect of the Zolgensma evaluation process.
“Zolgensma is not yet approved because its efficacy has not been established. The EMA has quite a significant number of questions for AveXis, and my understanding is that the EMA wants to very thoroughly review the data and the scope of approval,” he said. “I’d like it to come as soon as possible because there’s a very high unmet medical need in Europe.”
But even if the EMA gives Zolgensma the green light, getting the EU’s individual member countries to agree to cover patients’ costs for the $2.1 million treatment will be quite another story — no matter how good it may be for treating SMA.
Patryk Marczuk, scientific information coordinator of the Polish patient advocacy group Fundacja SMA, says that theoretically at least, Zolengsma is “everyone’s dream come true.” Yet he has doubts over both the therapy’s long-term effectiveness and EU governments’ willingness to pay for it.
“It’s like the holy grail of the search for a cure for SMA, because it’s a one-time shot and you’re set for your whole life,” said Marczuk, whose twin daughters, Gabriela and Patrycja, both have SMA type 3. “The first kids got the injection in 2015. So far, the drug is still working for those kids, but there’s still a question how it’s going to work in 10, 15 or 20 years. Hopefully, it will stay like it is right now.”
Zolgensma vs. Spinraza
The only other FDA-approved treatment for SMA is Spinraza (nusinersen), an injectable medication developed by Biogen. At a retail price of $750,000 for the first year of treatment and $375,000 each year after, Spinraza is already being used to treat more than 6,600 SMA patients around the world, including some 4,000 outside the United States.
SMA Europe, which is based in the U.K., said it’s “delighted” with the FDA’s approval of Zolgensma “as there are now two approved treatments” for the muscle-wasting disease.
“Members of SMA Europe have been working hard with AveXis to ensure the patient voice was taken into account while the drug was in development. It now anxiously awaits a decision from the EMA and further development of the intrathecal formulation to address the needs of older patients,” it stated in a May 24 note on its website.
 “We acknowledge there is still a long road to walk before European patients can access this new treatment,” it continued. “SMA Europe would regard it as unethical if the price would preclude any patient in any country from receiving this potentially lifesaving therapy.”
“We acknowledge there is still a long road to walk before European patients can access this new treatment,” it continued. “SMA Europe would regard it as unethical if the price would preclude any patient in any country from receiving this potentially lifesaving therapy.”
Yet Doug Henderson, managing director of the British patient advocacy group Spinal Muscular Atrophy UK, is skeptical about his government’s ability or willingness to pay for Zolgensma.
That’s because it only agreed to reimburse for Spinraza this May, after a long, bruising battle that led to a number of street protests against England’s National Institute for Health and Care Excellence (NICE).
“We are immensely excited about the prospects of a gene therapy for SMA. It’s a single dose which seems to imply life-changing results,” said Henderson, estimating that the disease affects anywhere from 800 to 1,400 people in Britain.
“Zolgensma is far more expensive, but if you look 10 years ahead and compare Spinraza versus a one-time gene therapy, it’s a no-brainer what will end up being cheaper over time,” he said. “The difficulty at the moment is to unblock the assessment system in this country. It just shows how behind we’ve become.”
EU-wide Spinraza coverage by 2024?
Rucinski told SMA News Today that a large proportion of Europeans still have no access to Spinraza, and that four of the EU’s 28 member states — Bulgaria, Estonia, Ireland, and Latvia — still have not agreed to make the therapy available through public healthcare.
To see the exact status of Spinraza access in each country, please click here for a detailed map.
“In Europe, the approval was for the entire spectrum of SMA, but Biogen did not have supporting data. This later caused trouble during the health technology assessment process because the regulators were unable to come up with reliable numbers to carry out calculations of cost-effectiveness,” Rucinski said.
“So for Zolgensma, pricing all depends on what AveXis proposes,” he continued. “For example, if we get a very broad label for Zolgensma and the company files separately for reimbursement in every country, then a huge number of patients will be included, and for many populations there will be no data. It will be very difficult to calculate the cost of intervention, how much these people would improve, whether they’d improve more than with Spinraza or less, or whether they’d improve at all.”
Arndt Rolfs, CEO of Centogene, said that in Germany, any doctor can prescribe Spinraza without having to go through committees — making the country a lucrative market for the injectable therapy.
“Spinraza is now at the second level of reimbursement, but the likelihood it will reach the highest level is close to 100 percent. The data is rather convincing,” he said, adding that “in Europe, if one EU member has reached the highest level of reimbursement, then all EU members have to follow that rule within three years.”
Rolfs, a neurologist, started Centogene 12 years ago and has headed the company since 2013. He predicted that “within the next five years, all EU countries will most likely approve reimbursement of Spinraza for all types of SMA.”
A key consideration of Spinraza over Zolgensma is that it is still a traditional pharmaceutical.
“Gene therapy needs a completely different solution,” he said. “You would never put $2 million on the table when you don’t know if the patient might change after three months to another insurance company. That’s the difficulty.”
Rolfs added: “I was one of the guys who was involved in one of the first gene therapy trials, and we realized that efficiency was going down after a few months. No one has ever proven that gene therapy would last for 10 years. We always see fading effects in terms of silencing the gene.”
Ultimately, he said, it comes down to whether taxpayers are willing to basically cure an SMA patient at the cost of putting many other people in danger.
“If you have €1,000 and you can save the lives of 99 patients suffering from cancer, or the life of one patient with a rare disease, it’s at least understandable that the government argues in the direction of saving the 99 patients with cancer. At the end of the day, the decision is a political and ethical one — but not a medical one.”





