Discussion
Discussion
FAQs about types of SMA
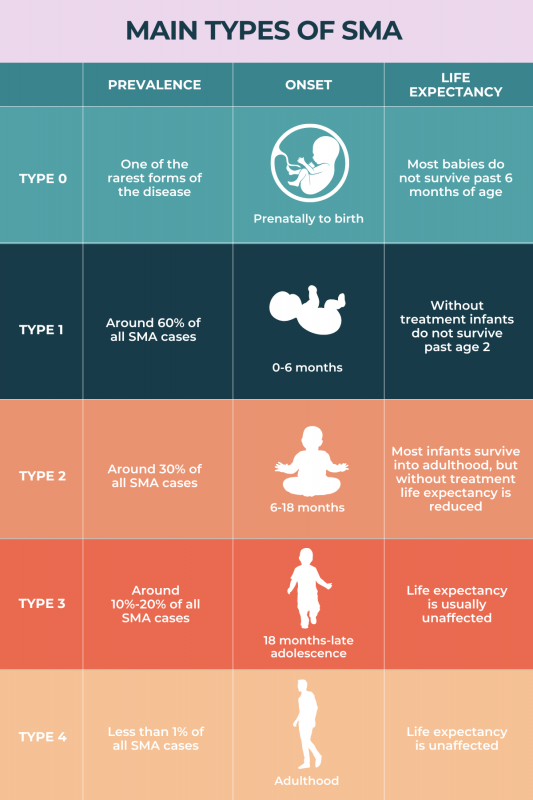
Figuring out what type of spinal muscular atrophy (SMA) someone has is done by combining clinical observations of a patient’s symptoms and age at onset, with genetic testing that identifies disease-causing mutations. For people with one of the five main SMA types, testing of SMN2 copy number also can help determine the disease type.
The most common form of spinal muscular atrophy (SMA) is type 1 disease, which accounts for about 60% of cases. SMA type 1 symptoms usually develop within an infant’s first 6 months of life.
Type 0 spinal muscular atrophy (SMA), also known as prenatal SMA, is generally considered to be the most severe form of the disease. This form is characterized by severe muscle weakness and breathing difficulties that develop while a fetus is still in the womb and are present and severe from birth.
 Medically reviewed by
Medically reviewed by