Mitochondria is a potential target for SMA treatment: Study
Exercise, urolithin A used to improve mitochondrial health in mice, cells
The parts of cells that produce energy, called mitochondria, in the skeletal muscles involved in voluntary movements don’t work properly in spinal muscular atrophy (SMA) and may contribute to the disease’s symptoms, a study in mice and cells suggests.
Engaging mice in a single session of exercise or adding urolithin A, a compound that promotes mitochondrial function, to lab-grown human cells led to benefits such as increased oxygen use, a sign that more energy is being produced. These findings suggest “lifestyle-based and pharmacological interventions may be effective countermeasures targeting [mitochondria] for therapeutic remodeling in SMA,” wrote researchers in Canada.
The study, “Skeletal Muscle Mitochondrial and Autophagic Dysregulation Are Modifiable in Spinal Muscular Atrophy,” was published in the Journal of Cachexia, Sarcopenia and Muscle.
SMA is chiefly caused by mutations in the SMN1 gene that result in a shortage of SMN, a protein needed for the maintenance of motor neurons, that is, the nerve cells that control voluntary movements. Without SMN, motor neurons die, causing progressive muscle weakness.
Mitochondria are small structures inside cells that act as their powerhouses, producing energy in the form of adenosine triphosphate (ATP), which they generate through a process called oxidative phosphorylation (OxPhos), which occurs in the mitochondrial inner membrane.
Improving mitochondrial health to treat SMA
This energy is crucial for skeletal muscle cells, which need large amounts of ATP to function properly. In SMA, mitochondria may not work efficiently, contributing to muscle weakness. To understand how SMA affects mitochondria, the researchers used genetically modified mice that mimic the disease.
They studied the mice at different stages of disease progression — before symptoms appear, and early symptomatic and late symptomatic stages. By analyzing their skeletal muscles, they determined how mitochondria change over time in response to the disease.
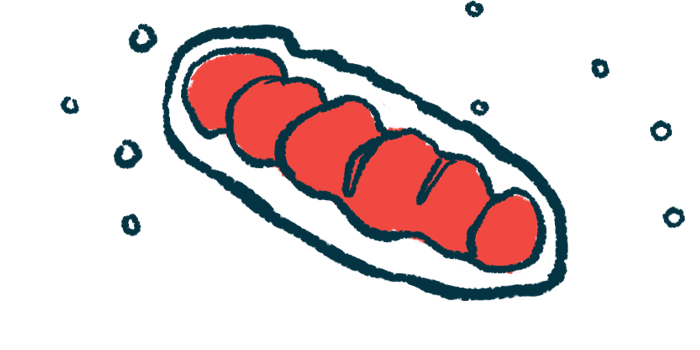
The levels of OxPhos proteins remained stable in mice with SMA. However, genes involved in mitochondrial synthesis and recycling were more active, or upregulated, in late-stage SMA, suggesting the body attempts to compensate for mitochondrial dysfunction by increasing the production of mitochondrial components.
Muscle cells of the mice with SMA had excessive autophagy, a process wherein cells break down and recycle damaged components. The presence of high levels of molecules like BCL2, interacting protein 3, and Parkin, which mark damaged mitochondria for degradation, suggested impaired clearance of damaged mitochondria in both early and late symptomatic stages. Also, mitochondrial fragmentation — where mitochondria break into smaller pieces — was observed. This is often a sign of dysfunction.
To test treatments, the researchers used two interventions: exercise and a compound called urolithin A. A single session of exercise helped improve mitochondrial health in mice by increasing citrate synthase, an enzyme involved in energy production, and reducing excessive autophagy.
In muscle cells from patients with SMA, urolithin A improved mitochondrial function by increasing the levels of OxPhos proteins and oxygen consumption, suggesting it restored mitochondrial health.
This study suggests the potential of targeting mitochondria to treat SMA. Lifestyle interventions like exercise, combined with pharmacological interventions like urolithin A, may offer promising strategies to improve mitochondrial health.