Scoliosis and treatment
Last updated Jan. 27, 2025, by Andrea Lobo, PhD

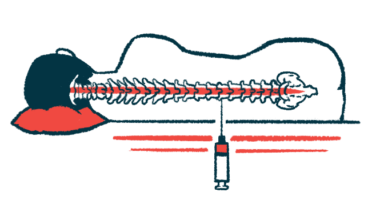
Scoliosis refers to an abnormal, sideways curvature of the spine. The condition may be caused by weakness in the muscles of the back that support the spine.
Signs of scoliosis may be marked by uneven shoulders and legs, elevated hips, leaning constantly to one side, shoulder blades that stick out, and a head not centered above the pelvis. The condition may lead to reduced mobility and functional impacts, particularly affecting the use of the arms. Respiratory problems due to reduced room for the lungs to expand may also occur.
Scoliosis in SMA
Spinal muscular atrophy (SMA) is a rare condition that’s mostly caused by mutations in the SMN1 gene, which lead to a deficiency of a protein called survival motor neuron, or SMN. The disease is characterized by progressive muscle weakness and atrophy, or wasting, that affect motor function and may cause problems with speaking, swallowing, and breathing.
Scoliosis is a common symptom of SMA, affecting as many as 90% of patients and occurring in different sections of the spine. It commonly develops from an early age, and progressively worsens.
Individuals with SMA type 1 and type 2, the most common forms of SMA, are particularly prone to scoliosis. Progression of this type of curvature is slower in patients with milder forms of the disease and in those able to walk.
SMA patients may also have an inward curve of the spine, known as lordosis, or a forward curvature of the spine, called kyphosis.
Scoliosis may be diagnosed in people with SMA by a visual examination in which a healthcare provider looks at posture, alignment, and spine curvature while the child or adolescent is standing or bent forward. X-rays of the spine are usually performed to confirm the diagnosis and reveal the severity of the scoliosis.
Scoliosis treatment
Treatment of scoliosis may include wearing a brace to help support the spine, and/or surgery to help correct the abnormal curvature, improve mobility, and preserve respiratory function.
Braces
Although wearing a brace does not prevent the development of scoliosis, it may help support the trunk while easing positioning and pain. Wearing a brace can sometimes improve the quality of life for a patient. Some specialists believe wearing braces may help slow curvature progression and delay surgery.
Braces are usually recommended to patients who are still growing and have a spine curvature greater than 25 degrees. Several types of braces are available, and one is chosen based on the patient’s degree of curvature and age:
- The Boston brace, a common brace designed for full-time wear, features molded, corrective pads and trim lines. The pads work to apply corrective pressure on the outer side of the curve, allowing the spine to align by also creating areas of relief on the inner side.
- The Milwaukee brace consists of a neck ring, pads, a plastic pelvic girdle, aluminum uprights, and metal bars in the front and the back. It’s used full-time in patients with curvatures that are higher in the thoracic or cervical sections of the spine.
- The Wilmington brace is a custom-fitted, jacket-style brace based on a cast. It is completed after adding corrective forces tailored to the patient’s spinal curvature.
- Nighttime braces, including the Charleston bending brace and the Providence brace, both apply corrective forces on the spine while the patient is lying down.
Surgery
At some point in spine curvature progression, surgery may be recommended, particularly in patients older than 10 and with a curvature greater than 40 degrees. Surgery may help stabilize the spine, improve balance and mobility, and ease pain, as well as preserve respiratory function and improve the patient’s quality of life.
In some cases, surgery has been reported to reduce functional abilities such as head movement. It also has been associated with complications including blood loss, pain, respiratory issues, infections, and nerve damage.
Several surgical procedures are available for scoliosis. The severity and location of the curvature, along with the patient’s age and pulmonary function, are factors that help determine which procedure is conducted. Combining different types of surgery is a possibility.
Spinal fusion
Spinal fusion involves the permanent connection of two or more vertebrae, which are the bones that form the spine, eliminating motion between them. The technique entails placing a bone or bone-like material in the space between two vertebrae. While the fusion occurs — a process that may take several months — rods, screws, or plates may be used to hold the vertebrae together.
Because fusion prevents further growth of the spine, it can only be performed once a patient has stopped growing. In the case of SMA, spinal fusion is only recommended for patients older than 10 who are unable to walk. The procedure is usually effective in correcting spinal curvature in 6-12 months.
Spinal fusion is the most invasive option, and it can be associated with back pain and declines in back and neck mobility.
Growing rods
Growing rods are expandable devices that are attached to the top and base of the spine using screws and hooks. Every six to nine months, surgery is needed to lengthen the rods. For that reason, the surgery can be performed in younger children with spine curvatures greater than 40 degrees.
Magnetically controlled growing rods, approved in Europe and Asia but not in the U.S., allow adjustment of such rods in outpatient care, without the need for follow-up surgeries after the initial procedure.
Vertical expandable prosthetic titanium ribs (VEPTR)
In this procedure, rods are attached to the ribs or the spine to help straighten the spine and separate the ribs, with a goal of preventing deterioration of breathing function. It is an option for younger children with spine curvatures greater than 40 degrees.
Both growing rods and VEPTR may require spinal fusion later in life, and the devices may loosen after surgery.
SMA News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Spinraza treatment improves motor function for adults with SMA: Study
- Why the disability representation in ‘The Beauty’ is a hot mess
- Scholar Rock to resubmit application for SMA therapy apitegromab to FDA
- Today is a good day for me to show appreciation to my caregivers
- Ahead of this year’s MDA Conference, association’s CEO speaks of ‘hope’